Back to Journals » Therapeutics and Clinical Risk Management » Volume 20
Comparison Study Among Three Surgical Methods in the Treatment of Isolated Fractures of the Greater Tuberosity of the Humerus
Authors Tao F, Li L, Wang D, Dong J, Zhou D, Song W
Received 17 December 2023
Accepted for publication 15 July 2024
Published 9 August 2024 Volume 2024:20 Pages 483—493
DOI https://doi.org/10.2147/TCRM.S455379
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Fulin Tao,1,* Lin Li,2,3,* Dawei Wang,1,2 Jinlei Dong,1 Dongsheng Zhou,1,2 Wenhao Song1,2,4
1Department of Orthopedic Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, People’s Republic of China; 2Department of Orthopedic Surgery, Shandong Provincial Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, People’s Republic of China; 3Department of Orthopedic Surgery, Tengzhou Central People’s Hospital Affiliated to Jining Medical University, Tengzhou, Shandong, People’s Republic of China; 4Shandong Yuhuang Chemical Co., Ltd, Heze, Shandong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenhao Song, Department of Orthopedic Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, People’s Republic of China, Email [email protected]
Introduction: This study aimed to compare the efficacy of three methods for isolated greater tuberosity fractures of the humerus.
Methods: A retrospective review of patients with isolated humeral greater tuberosity fractures between January 2013 and June 2021 in our institution. We recorded data on patient demographics, injury characteristics, preoperative and postoperative imaging findings, length of incision, operative time, and intraoperative blood loss.
Results: A total of 107 patients met the inclusion criteria and were divided into three groups. 50 patients in group A were administered a proximal humeral internal locking system (PHILOS) plate fixed using the deltopectoral approach, 26 patients in group B were administered a PHILOS plate fixed using the deltoid-splitting approach, and 31 patients in group C were administered a novel anatomical plate fixed using the deltoid-splitting approach. No significant differences were identified in sex, age, injury mechanism, type of fracture, dominant side limb, or shoulder anterior joint dislocation. However, the operative time, blood loss, and the length of incision was shorter than in Group C. Moreover, pain was evaluated on the third and fifth days after surgery; pain was lower in Group C, and pain at the last follow-up was not different between the groups. No significant differences were identified in the Constant score, DASH score, and ROM at the last follow-up. 2 patients were diagnosed with subacromial impingement, 1 in Group A one in Group B, and 1 patient in Group B experienced axillary nerve injury after surgery.
Conclusion: The novel anatomical plate fixed using the deltoid-splitting approach can achieve good results in the treatment of isolated humeral greater tubercle fractures with less blood loss, shorter operative time, and shorter surgical incisions, and can relieve pain in the early postoperative period.
Keywords: PHILOS plate, a novel anatomical plate, deltopectoral approach, deltoid-splitting approach, greater tuberosity fracture of humerus
Background
Proximal humerus fractures are common injuries in the upper extremity, and isolated greater tuberosity fractures account for approximately 20% of all proximal humeral fractures.1,2 The most common indication for nonsurgical treatment of isolated greater tuberosity fractures is ≤5 mm of displaced fragments, and it is also accepted that fragments displaced >5 mm are considered for surgical treatment.3,4 Park recommended that displacement is >3 mm should be treated by surgical fixation in athletes or overhead workers.5 There are several fixation techniques to treat greater tuberosity fractures, including screw fixation, plate fixation, tension banding, transosseous suture, and arthroscopic double-row suture anchor fixation. According to biomechanical experiments, many surgeons believe that plate fixation is a more effective method, especially in elderly patients with osteoporosis.6
The commonly used plate is the proximal humerus internal locking system (PHILOS) plate. There are two common approaches for open reduction and internal fixation of isolated greater tuberosity fractures: the deltopectoral approach and the deltoid-splitting approach, which is called the minimally invasive plate osteosynthesis (MIPO) technique. Because the PHILOS plate is relatively long, the deltopectoral approach is most commonly used. However, this approach may have shortcomings, such as excessive exposure and significant scarring. This can cause additional pain and a psychological burden to the patient. Therefore, some surgeons have attempted the deltoid-splitting approach because of its special anatomical structure, and some patients had symptoms of axillary nerve injury.7,8 Related cadaveric experiments also confirmed that the deltoid-splitting approach could increase the risk of axillary nerve injury.9 In recent years, with the development of internal fixation systems, a novel anatomical plate of the greater tuberosity was designed. This plate is smaller than other available PHILOS plates available and is specifically used for the treatment of greater tuberosity fractures. It can completely cover the greater tuberosity and fix fragment rigidly.10 This also provides an opportunity for the safe adoption of the deltoid splitting approach. However, there is a lack of relevant studies. The main objective of this study was to compare the efficacy of the three surgical methods in the treatment of isolated fractures of the greater tuberosity of the humerus.
Patients and Methods
We retrospectively analyzed all patients with isolated greater tuberosity fractures who were treated at our institution between January 2013 and June 2021. Permission for this study was obtained from the Medical Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong First Medical University.
Inclusion and Exclusion Criteria
The inclusion criteria in this retrospective study were as follows: 1) patients were diagnosed with greater tuberosity fracture on radiological examination; 2) age > 16 years; 3) time from injury to operation less than three weeks; 4) fragments fixed by plate (PHILOS plate or novel anatomical plate); 5) no previous shoulder joint injury or surgery; and 6) patients with a follow-up time >12 months.
The Exclusion criteria were as follows: 1) age ≤ 16 years; 2) open fracture; 3) combined vascular and nerve injury; 4) time from injury to operation more than three weeks; 5) non-operative treatment.
Data Collection
The patients were divided into three groups according to the surgical method. We collected the following data for each patient: sex, age, fracture type, cause of injury, shoulder joint dislocation (yes or no), dominant limb (yes or no), surgical method, time of operation, blood loss, length of incision, rotator cuff injury (yes or no), days of hospital stay, and follow-up time. Several classifications exist for greater tuberosity fractures. We used the Mutch system to classify bony injuries. Briefly, three fracture types were described: avulsion, split, and depression.11
Surgical Procedure
All patients were performed general anesthesia and were placed in a beach chair position.
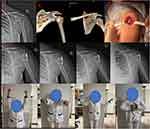
Group A (PHILOS plate fixed using the deltopectoral approach): A skin incision was made from the coracoid process and extended to the middle and distal ends of the deltoid. The cephalic vein was separated and pulled laterally to expose the space between the deltoid and the pectoralis major. The shoulder joint was rotated to expose the fragment, clear the hematoma, and reduce the fragment, and the fragment was fixed with a PHILOS plate (DePuy Synthes, West Chester, PA, USA) (Figure 1A).
 |
Figure 1 (A) PHILOS plate fixed by deltopectoral approach. (B) PHILOS plate fixed by deltoid-splitting approach. (C) A novel anatomical plate fixed by deltoid-splitting approach. |
Group B (PHILOS plate fixed using the deltoid-splitting approach): A skin incision was made from the acromion and extended less than 5 cm. The deltoid fibers were split at the juncture of the anterior and middle deltoids. The deltoid was split by less than 4–5 cm, and care was taken to avoid axillary nerve injury. After the greater tuberosity of the humerus was exposed, the hematoma was cleared, the fragment was reduced, and a K-wire was used to fix the fracture fragment temporarily. The index finger, introduced into the rent of the deltoid, cleared the space between the deltoid and the bone. The axillary nerve is perceived as a cord-like structure at the deep aspect of the deltoid and is protected by the index fingertip during manipulation through the proximal window. A distal lateral skin incision of 2 cm was made, approximately 4 cm from the proximal incision. A PHILOS plate (DePuy Synthes, West Chester, PA, USA) was inserted from proximal to distal and used to fix the fragments (Figure 1B).
Group C (a novel anatomical plate fixed by the deltoid-splitting approach): As previously mentioned in group B, a proximal incision was used to expose the fragment, a distal incision was not required, and a novel anatomical plate (Double Medical Technology Inc., Xiamen, China) was used to fix the fragments (Figure 1C).
Intraoperative radiographs were used to elevate the quality of fracture reduction, and the rotator cuff was explored and repaired if there were any injuries. Antibiotics were routinely administered 24 h after surgery. For the first three weeks, all patients suspended their upper limbs and underwent mild passive activities. After 3 weeks, the patient was encouraged to participate in activities of daily living, such as washing the face, brushing teeth, and combing hair. Active shoulder training was initiated at 6 weeks. Intensive exercise was permitted from 12 weeks.
Follow-Up and Postoperative Evaluation
Patients were followed-up in the outpatient clinic at 1, 3, and 6 months after surgery and every 6 months thereafter. Radiographs were used to evaluate the radiological outcomes after surgical treatment. Complications including infection, axillary nerve injury, shoulder redislocation, skin numbness, loss of reduction, and implant loosening were also documented. The visual analog scale (VAS) score system was used to evaluate pain at the third, fifth, and last follow-up. The Constant score was used to evaluate the shoulder function at the last follow-up. The Constant score results were categorized as excellent (86–100), good (71–85), moderate (56–70), and poor (0–55). We also used the Shortened Disabilities of the Arm, Shoulder and Hand Questionnaire (Q-DASH) score, a 30-item, self-reported instrument, to evaluate the physical function of the upper limb at the last follow-up. DASH score was graded as excellent (0–24), good (25–49), moderate (50–74), or poor (75–100). At the final follow-up, ROM including forward flexion, abduction, and external rotation at the neutral position were measured, whereas internal rotation was determined using the vertebral-level method (Figures 2–4).12 Radiographs and functional evaluations were performed by two experienced musculoskeletal surgeons who did not participate in the surgeries. Both observers achieved an exact agreement when evaluating all images. Complications were observed in all the patients.
Statistical Analysis
The data were initially analyzed using descriptive statistics (mean ± SD or absolute value and percentage). For continuous data, only parameter-free testing (Mann–Whitney U-test or Wilcoxon signed-rank test) was used because of the small sample size and the presence of outliers. The chi-square test was used to compare count data, and the one-way ANOVA test was used for multiple comparisons. A two-sided significance value of 0.05 was used for all statistical tests. All statistical analyses were performed with SPSS Statistics (Version 28.0; IBM).
Results
During the study period, 107 patients with isolated greater tuberosity fracture were treated at our institution. Fifty patients were treated with the PHLIOS plate using the deltopectoral approach (Group A), 26 patients were treated with the PHILOS plate using the MIPO technique (Group B), and 31 patients were treated with a novel anatomical plate using the deltoid-splitting approach (Group C). There were 31 males and 19 females in Group A, 17 males and 9 females Group B, and 20 males and 11 females in Group C; the ratios were similar. The average age was 43.94±10.73, 42.92±7.25 and 43.84±8.80, respectively. The primary mechanism of injury falls in all groups, accounting for 50%, 50%, and 45% of the cases. Most of the patients had injuries on the dominant side. 16% (n=8), 15% (n=4), and 16% (n=5) of patients had combined shoulder joint dislocations, all of which were anterior dislocations. According to the Mutch system, split fractures are the most common type of fracture. There were no significant differences among the three groups in terms of average age, sex composition, mechanism of injury, dominant limb, shoulder joint dislocation, and type of fracture. The epidemiological data are summarized in Table 1.
 |
Table 1 Demographic Data |
In the record, the operative time for Group A was 64.81±6.72 min, with blood loss of 88.08±16.18 mL, length of incision was 15.35±0.68 cm. The operative time for the Group B was 61.82±4.41 min, with blood loss of 83.64±16.66 mL, length of incision was 9.27±0.96 cm. The operative time for the Group C was 50.38±4.58 min, with blood loss of 55.38±10.09 mL, length of incision was 4.54±0.50 cm. There was a significantly shorter operative time, less blood loss, and shorter incision length in Group C than other two groups. There were no significant differences in hospital stay and follow-up time between the three groups. The numerically obtained data are presented in Table 2.
 |
Table 2 Surgical Related Data |
The VAS scores on third day after operation was 7.0±0.62 in Group A and 6.64±0.64 in Group B, with significant difference. On the fifth day, the VAS score was 6.38±0.60 in Group A and 5.55±0.50 in Group B, there was significant differences between ± two groups. The VAS score on the third and fifth day after operation was 5.54±0.75 and 3.85±0.66 in Group C, it was significantly lower than the other two groups. However, VAS scores at the final follow-up were not significantly different. The function of the shoulder joint was also evaluated, and the Constant scores were 92±7.11 in Group A, 91.09±7.56 Group B and 92.38±5.99 in Group C, there was no significant difference observed between the three groups. The DASH scores were 2.94±3.19, 3.11±1.82 and 3.02±1.77, respectively, with no significant difference between the three groups. The mean active forward flexion was 157.92±15.11, 156.18±20.63 and 156.46±19.71 degrees, the mean abduction was 145.62±28.12, 144.09±18.07 and 143.38±17.0 degrees, the mean external rotation in the neutral position was 45.38±9.40, 45.91±7.93 and 45.77±7.81 degrees, there were no significant difference between three groups. The mean internal rotation increased to the 11th thoracic vertebral level (from L5 to T7). The data on pain and functional evaluations are presented in Table 3.
 |
Table 3 Pain and Functional Evaluation |
Complications were also observed, and all the patients achieved good incision healing without infection. There were no cases of shoulder redislocation, skin numbness, loss of reduction, or implant loosening. Two patients were diagnosed with subacromial impingement: one in Group A one in Group B; they refused surgical treatment. One patient in Group B experienced axillary nerve injury after surgery and recovered after three months of nerve treatment.
Discussion
Isolated greater tuberosity fractures are common shoulder joint injuries, accounting for approximately 20% of all proximal humeral fractures.1,2 This injury is often accompanied by shoulder dislocation and rotator cuff injury.1,13 Serving as attachment points of the rotator cuff, the greater tuberosity plays an important role in the motion of the shoulder joint; therefore, the treatment of greater tuberosity fractures is a hot topic. In previous studies, inappropriate treatment for greater tuberosity fractures often resulted in shoulder disability due to subacromial impingement and limitations of abduction and external rotation.14,15 It is generally accepted that fractures displaced >5 mm require surgical treatment, and the goal of surgical treatment is restoration of normal anatomy with stable fixation that permits early functional exercises and preserves the integrity of the rotator cuff.15
There is no gold standard for fixing fragments of the greater tuberosity. There are various methods of fixation, such as screw fixation, tension banding, transosseous suturing, plate fixation, and arthroscopic double-row suture anchor fixation. According to the mechanism of injury, Mutch classified greater tuberosity fractures into three types, type I was avulsion fracture, type II was split fracture, and type III was depression fracture.11 Mutch also considered that plate fixation was appropriate for split fractures and tension bands for avulsion fractures.11 Based on biomechanical experiments, Gaudelli et al6 found that locking plate fixation could provide superior fixation of humerus split type greater tuberosity fractures than tension bands and double row suture bridges. In addition, with wide pressure distribution over a relatively larger area, the plate can effectively fix fragments, especially split fracture fragments.10
In clinic, the most common plate used to fix the greater tuberosity fractures is PHILOS plate, which is designed to fix proximal humerus fractures. This plate can achieve good results in the fixation of greater tuberous fractures, and we obtained the same results in this study. Fracture union was achieved in all patients in groups A and B without loosening of the plate or fragment displacement. However, the PHILOS plate is too large and difficult to place, and the deltopectoral approach is generally used, which results in large surgical trauma and a large stripping range. This traditional approach also causes additional soft tissue damage and deltoid muscle injury and is not conducive to early functional exercise after surgery.
Therefore, in recent decades, the deltoid-splitting approach has become a popular treatment for proximal humerus fractures.16,17 This is a minimally invasive plate osteosynthesis technique that has the advantages of less soft stripping and direct visualization of the greater tuberosity. Compared with the deltopectoral approach, the deltoid-splitting approach can be achieved with minimal invasion, less bleeding, and less pain to facilitate early functional exercise. In this study, we obtained the same results: the average VAS score was significantly lower than that of the deltopectoral approach on the third and fifth day after operation, the incision length was shorter, and blood loss was less than that of the deltopectoral approach. We treated 26 patients using the deltoid-splitting approach, and achieved fracture union and excellent outcomes in all patients with isolated greater tuberosity fractures.
The axillary nerve is at risk when using the deltoid splitting approach. It is located approximately 6 cm distal to the acromion; therefore, the proximal incision must be shorter than 5 cm.18 In general, a suitable tunnel must be prepared beneath the nerve and the PHILOS plate must be inserted gently. Some surgeons recommend the complete exposure of the axillary nerve by extending the anterolateral incision. However, there is still a risk of injury because the axillary nerve has many branches in this region.19 Traver JL did a cadaveric experiment and found that strain placed across the nerve with retraction could lead to micro-trauma, a risk of neuropraxia.9 Gönç t al8 treated 31 patients with proximal humerus fracture by deltoid-splitting approach and one case suffered axillary nerve injury. We treated 26 patients with isolated greater tuberosity fracture by deltoid-splitting approach, one patient suffered axillary nerve and finally recovered. Therefore, more effective and safer treatments are required for greater tuberosity fractures.
Because of the disadvantages of the PHILOS plate, surgeons have attempted to use other plates to treat greater tuberosity fractures. Chen et al20 used AO X-shaped midfoot locking plates to treat 19 patients with isolated greater tuberosity fractures and achieved fracture healing without any complications. Schöffl et al4 used a self-adjusted calcaneus plate to treat ten patients and obtained excellent postoperative outcomes. Lee21 and Yin22 reported that the hook plate could provide sufficient stability and lead to satisfactory clinical outcomes for isolated greater tuberosity fractures. However, these plates are not specifically designed to fix greater tuberosity fractures and need to be shaped in advance.
In recent years, a new low-profile anatomical locking plate was designed to fix isolated greater tuberosity fracture.10 As previously introduced in the literature, this plate has several advantages in the treatment of isolated greater tuberosity fractures.10 The plate is short enough and can be placed intact by the deltoid-splitting approach. In this study, the length of incision was minimally invasive (average, 5 cm) and significantly shorter than that in the other two groups. The risk of axillary nerve injury is also reduced because the incision is shorter and the plate does not pass through the deep surface of the axillary nerve. Meanwhile, due to the small incision and small trauma, the pain of the patients on the third and fifth days after surgery was significantly lower than that in the other two groups, and functional exercise could be performed early. In addition, a previous study revealed that the larger the implant, the greater the chance of impingement.23–25 This plate is thinner than the PHILOS plate (approximately 1 mm thick), which can effectively reduce the possibility of acromial impingement. In our study, we also found two patients with subacromial impingement after treatment with a PHILOS plate (one in Group A and one in Group B) and none in Group C. This is an anatomical plate that can fix fragments more firmly, and all patients treated by this plate achieved fracture healing and no loss of reduction or implant failure occurred. The postoperative outcomes were similar to those in the other two groups.
In the treatment of isolated greater tuberosity fractures with the novel anatomical plate, our experience was as follows: (1) Because the axillary nerve is at the deep surface of the deltoid, 6 cm below the acromion, the length of the incision should be no longer than 5 cm. A suture was made at the distal end of the deltoid muscle during the incision to avoid excessive traction, leading to further tear of the deltoid muscle and injury to the axillary nerve. (2) The greater tuberosity fracture fragment is usually thin and displaced posteriorly and upward by the rotator cuff. Fracture fragments should be avoided during reduction, and suture of the rotator cuff combined with rotation of the humerus can be used for indirect reduction. (3) For osteoporotic fractures, plate fixation combined with transosseous sutures is recommended to reduce the risk of postoperative fracture displacement.
The current study has some limitations. First, our study was retrospective rather than prospective. A small number of patients were included in the study because of the low morbidity associated with isolated greater tuberosity fractures. Future multicenter, large-sample, adequately powered, randomized controlled trials are needed to assess the efficacy of these interventions. Long-term follow-up is required to assess the complication rates of this surgical technique.
Conclusion
Isolated greater tuberosity fractures fixed with a novel anatomical plate using the deltoid-splitting approach could reduce intraoperative blood loss, shorten operation time, relieve postoperative pain, and achieve good clinical results, demonstrating that this surgical method is a safe and effective option for treating isolated greater tuberosity fractures.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethical Statement and Informed Consent
The experimental protocol was established according to the ethical guidelines of the Declaration of Helsinki and was approved by the Human Ethics Committee of Shandong Provincial Hospital Affiliated to Shandong First Medical University. Written informed consent was obtained from all the participants.
Consent for Publication
The corresponding author declares that this article is of original material, that is, it is not currently submitted elsewhere for editing, review, or publication, and has not been published elsewhere. In addition, this study did not duplicate previously published materials. The corresponding author agrees with the publication of this article.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81672156), National Natural Science Foundation of China (No. 81972057) and Natural Science Foundation of Shandong Province (No. ZR202211190047).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005;10(5):441–444. doi:10.1007/s00776-005-0924-6
2. glesias-Rodríguez S, Domínguez-Prado DM, García-Reza A, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res. 2021;16(1):402. doi:10.1186/s13018-021-02551-x
3. Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008;65(4):843–848. doi:10.1097/01.ta.0000233710.42698.3f
4. Schöffl V, Popp D, Strecker W. A simple and effective implant for displaced fractures of the greater tuberosity: the ”Bamberg” plate. Arch Orthop Trauma Surg. 2011;131(4):509–512. doi:10.1007/s00402-010-1175-3
5. Park TS, Choi IY, Kim YH, et al. A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis. 1997;56(3):171–176.
6. Gaudelli C, Ménard J, Mutch J, Laflamme GY, Petit Y, Rouleau DM. Locking plate fixation provides superior fixation of humerus split type greater tuberosity fractures than tension bands and double row suture bridges. Clin Biomech. 2014;29(9):1003–1008. doi:10.1016/j.clinbiomech.2014.08.013
7. Knežević J, Mihalj M, Čukelj F, Ivanišević A. MIPO of proximal humerus fractures through an anterolateral acromial approach. Is the axillary nerve at risk? Injury. 2017;48(Suppl 5):S15–S20. doi:10.1016/S0020-1383(17)30733-7
8. Gönç U, Atabek M, Teker K, Tanrıöver A. Minimally invasive plate osteosynthesis with PHILOS plate for proximal humerus fractures. Acta Orthop Traumatol Turc. 2017;51(1):17–22. doi:10.1016/j.aott.2016.10.003
9. Traver JL, Guzman MA, Cannada LK, Kaar SG. Is the axillary nerve at risk during a deltoid-splitting approach for proximal humerus fractures? J Orthop Trauma. 2016;30(5):240–244. doi:10.1097/BOT.0000000000000492
10. Zeng LQ, Chen YF, Jiang YW, Zeng LL, Miao XG, Liang WG. A new low-profile anatomic locking plate for fixation of comminuted, displaced greater tuberosity fractures of the proximal humerus. J Shoulder Elbow Surg. 2021;30(6):1402–1409. doi:10.1016/j.jse.2020.08.036
11. Mutch J, Laflamme GY, Hagemeister N, Cikes A, Rouleau DM. A new morphological classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint J. 2014;96-B(5):646–651. doi:10.1302/0301-620X.96B5.32362
12. Han SH, Oh KS, Han KJ, Jo J, Lee DH. Accuracy of measuring tape and vertebral-level methods to determine shoulder internal rotation. Clin Orthop Relat Res. 2012;470(2):562–566. doi:10.1007/s11999-011-2112-7
13. Gillespie RJ, Johnston PS, Gordon VA, Ward PJ, Getz CL. Using plate osteosynthesis to treat isolated greater tuberosity fractures. Am J Orthop. 2015;44(8):E248–E251.
14. DeBottis D, Anavian J, Green A. Surgical management of isolated greater tuberosity fractures of the proximal humerus. Orthop Clin North Am. 2014;45(2):207–218. doi:10.1016/j.ocl.2013.12.007
15. White EA, Skalski MR, Patel DB, et al. Isolated greater tuberosity fractures of the proximal humerus: anatomy, injury patterns, multimodality imaging, and approach to management. Emerg Radiol. 2018;25(3):235–246. doi:10.1007/s10140-018-1589-8
16. Gardner MJ, Griffith MH, Dines JS, Lorich DG. A minimally invasive approach for plate fixation of the proximal humerus. Bull Hosp Jt Dis. 2004;62(1–2):18–23.
17. Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010;24(7):400–406. doi:10.1097/BOT.0b013e3181ccafb3
18. Esenyel CZ, Dedeoğlu S, Imren Y, Kahraman S, Çakar M, Öztürk K. Relationship between axillary nerve and percutaneously inserted proximal humeral locking plate: a cadaver study. Acta Orthop Traumatol Turc. 2014;48(5):553–557. doi:10.3944/AOTT.2014.13.0083
19. Aksu N, Karaca S, Kara AN, Işiklar ZU. Minimally invasive plate osteosynthesis (MIPO) in diaphyseal humerus and proximal humerus fractures. Acta Orthop Traumatol Turc. 2012;46(3):154–160. doi:10.3944/aott.2012.2592
20. Chen YF, Zhang W, Chen Q, Wei HF, Wang L, Zhang CQ. AO X-shaped midfoot locking plate to treat displaced isolated greater tuberosity fractures. Orthopedics. 2013;36(8):e995–e999. doi:10.3928/01477447-20130724-13
21. Lee WY, Shin HD, Kim KC, Cha SM, Jeon YS, Kim DH. Open reduction and stable internal fixation using a 3.5-mm locking hook plate for isolated fractures of the greater tuberosity of the humerus: a 2-year follow-up study using an innovative fixation method. Clin Orthop Surg. 2021;13(3):293–300. doi:10.4055/cios20212
22. Yin Q, Rui Y, Wu Y, et al. Surgical treatment of avulsion fracture around joints of extremities using hook plate fixation. BMC Musculoskelet Disord. 2019;20(1):200. doi:10.1186/s12891-019-2585-1
23. Niall DM, O’Mahony J, McElwain JP. Plating of humeral shaft fractures--has the pendulum swung back? Injury. 2004;35(6):580–586. doi:10.1016/j.injury.2003.10.021
24. Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg. 2010;19(4):489–494. doi:10.1016/j.jse.2009.09.005
25. Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA. Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury. 2008;39(3):306–313. doi:10.1016/j.injury.2007.10.011
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.