Back to Journals » International Medical Case Reports Journal » Volume 17
Congenital Rubella Syndrome: A Case Report from Somalia
Authors Ismail FA, Ali YK, Ali AM, Hirsi IM, Ali NA, Kassim MM , Ahmed FA, Ali MN
Received 5 April 2024
Accepted for publication 13 August 2024
Published 17 August 2024 Volume 2024:17 Pages 751—755
DOI https://doi.org/10.2147/IMCRJ.S472306
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Vinay Kumar
Farah Abdullahi Ismail,1 Yasir Khalif Ali,1 Ahmed Mohamed Ali,2 Ibrahim Mohamed Hirsi,1 Naima Abukar Ali,1 Mohamed Mukhtar Kassim,1 Farah Ali Ahmed,1 Mohamed Nur Ali1
1Pediatric Department of Mogadishu-Somalia Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia; 2Department of Infectious Diseases and Clinical Microbiology, Mogadishu-Somalia Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia
Correspondence: Farah Abdullahi Ismail; Ahmed Mohamed Ali, Email [email protected]; [email protected]
Abstract: Congenital rubella syndrome (CRS) is a serious condition with a high rate of morbidity. It is currently a rare disorder, especially in developed countries, because of universal vaccination campaigns. However, it remains a public health concern in developing countries. Here, we report a case of congenital rubella syndrome in a mother who did not receive any prenatal care or had a known history of vaccination. He is a term male infant, and the infant’s positive rubella IgM confirmed the diagnosis. The baby had a bilateral cataract, convulsions, Patent ductus arteriosus (PDA)-related cardiomegaly, and bilateral hearing loss. The only known preventive measure for congenital rubella syndrome is vaccination.
Keywords: congenital rubella syndrome, vaccine, prenatal care
Introduction
The rubella virus, which is part of the Rubivirus genus in the togaviridae family, is the infectious agent that causes rubella, German measles, or three-day measles.1
It can spread by direct contact with an infected person’s saliva or mucous, or it can spread through the air as a result of respiratory droplets released during a cough or sneeze.
Congenital rubella syndrome (CRS) arises when the developing fetus gets affected by the rubella virus in an infected mother, typically in the first trimester.2
There is currently no rubella vaccine available in Somalia to prevent congenital rubella syndrome (CRS), which is the result of a rubella infection. This is because there is no combination measles, mumps, and rubella (MMR) vaccine available in the country.
A woman has a 90% probability of infecting her fetus with rubella if she develops the virus in the early stages of her pregnancy.3 Sensorineural hearing loss is the most prevalent symptom. 58% of patients have some form of deafness, either unilateral or bilateral. Ocular disorders such as cataract, infantile glaucoma, and retinopathy affect 43% of the population. The most common findings are pigmentary rubella retinopathy and cataract.4
Congenital heart disease, which includes pulmonary arterial stenosis and patent ductus arteriosus, is another common manifestation.5
Hematological (thrombocytopenia and anemia), dermatological (rubelliform rash and blueberry muffins), intracranial/basal ganglia calcifications, hepatosplenomegaly, and metaphyseal lucencies in long bones are among the systemic findings in Congenital rubella syndrome (CRS).6
The challenging diagnosis of Congenital rubella syndrome (CRS) at this stage of life is due to its similarities with other congenital viral infections like Cytomegalovirus (CMV) and the limited awareness of the condition among pediatric and family medicine practitioners.7
Case Presentation
A full-term 35-day-old male infant was referred to us complaining of convulsions, fever, and bilateral congenital cataracts (Table 1).
 |
Table 1 Major Clinical Findings and Investigations |
Although not a high grade fever, the fever persisted and subsided after taking an antipyretic. In addition, he experiences episodes of clonic movement in his right leg, facial twitching, and abnormal body movements. Congenital cataracts and these complaints were since birth.
The baby was born by a 33 years old multigravida mother via a spontaneous vaginal delivery at a different hospital. The newborn was admitted to the neonatal intensive care unit after requiring oxygen therapy and resuscitation on delivery. On the thirty-fifth day, the patient was referred to us for an additional assessment and treatment.
No vaccinations or prenatal care were given to the mother during her pregnancy. The mother experienced skin rashes, headaches, and fever during the initial months of her pregnancy, but she did not seek medical attention at a hospital. She is the mother of three other healthy children. The mother’s drug history was limited to analgesics. The baby’s parents, who are consanguineous, had no record of inherited medical disorders. Upon examination, the baby appeared ill with generalized hypotonia, respiratory distress, and no signs of cyanosis.
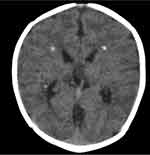
The patient’s vitals are: HR — 150 bpm, RR — 60 bpm, T — 37.6 OC, SPO2 — 94% in room air, blood sugar — 82 mg/dl, birth weight — 3.55 kg, height — 55 cm, and head circumference — 35.8 cm. The patient exhibited a pink conjunctiva, an anterior fontanel of 1.5×1.5 cm, bilateral cataractous lenses (Figure 1), and involuntary rolling of the eyes. His Chest or respiratory system: Intercostal retractions but has good air entry. Cardiovascular system: Continues machine like murmur at upper left sternal border. Abdomen: no abdominal distension and hepato-splenomegaly. Nervous system: baby was hypotonic but alert, had convulsions, and all of his reflexes were intact except the imperfect moro-reflex. According to the Investigations his full blood count (FBC) of the patient showed WBCs 9×1000/mm3, HB 16.6 g/dl and platelet count 181×1000/mm3, no thrombocytopenia was seen in all tests. The biochemical analysis revealed normal tests for the renal, liver, and thyroid functions, normal calcium, potassium, magnesium, and glucose levels but a slight decrease in sodium levels (129 mmol/l) and albumin (2.7g/dl). The C-reactive protein (CRP) measured 29 mg/l. The coagulation test results were unremarkable. The rubella IgM antibody level in the TORCH infections serology test was found to be elevated at 50.2 AU/mL (Table 1). The serology results were all negative for HSV, CMV, and toxoplasma. Unfortunately, we could not carry out PCR tests at our facility. The chest x-ray of the baby showed Cardiomegaly and mild bilateral lung infiltrates (Figure 2). An echocardiogram detected a low ejection fraction of 40% and a patent ductus arteriosus (PDA). The brain CT scan revealed periventricular calcifications (Figure 3) that were properly symmetric on both sides. Additionally, there was hypodensity in the white and grey matter of both hemispheres, which was related to a loss of differentiation between them. There was no significant meningeal or parenchymal enhancement.
 |
Figure 1 Infant with bilateral cataract. |
 |
Figure 2 X-ray chest (posterior anterior view) showing cardiomegaly and bilateral lung infiltrates. |
The ophthalmoscope reveals bilateral congenital cataracts. There was also bilateral sensorineural hearing loss. Initially, we began empiric intravenous antibiotics (ampicillin and cefotaxim). For the low EF of the previous echocardiography, he was given an enalapril tab and furosemide; however, we stopped after the patient’s ejection fraction (EF) improved. Since birth, he has been taking phenobarbital, which was prescribed at the time of discharge. The ophthalmology department suggested an upper level clinic for the operation of the congenital cataract.
After six days of clinical improvement and satisfactory oral intake, the patient was discharged home with surgical arrangements for treating congenital cataracts and Patent ductus arteriosus (PDA).
Discussion
Congenital rubella syndrome (CRS) arises when the developing fetus gets affected by the rubella virus in an infected mother, typically in the first trimester.2 The variety of systemic involvement includes progressive encephalopathy in infancy and childhood, sensorineural deafness, and acute multiorgan dysfunction in neonates.4 The severity of abnormalities is determined by the gestational age at the moment of exposure and the teratogenicity of the virus.4 Our patient’s mother experienced a viral exanthema during her first trimester of pregnancy, followed by a brief fever and headache, which strengthened our suspicions. The World Health Organization has defined diagnostic criteria. Congenital rubella syndrome (CRS) can be identified in the postnatal period using a classical triad of clinical signs (congenital heart disease, cataracts, and sensorineural hearing loss). Rubella virus identification (in newborn oropharyngeal secretions and urine), retrieval of rubella-specific IgM antibodies from either the neonatal blood or cord blood, and regular evaluation of elevated rubella IgG titers are the methods of diagnosis for the disease.8 Our patient’s congenital rubella syndrome diagnosis was confirmed by an elevated IgM level. Currently, there is no approved treatment for Congenital rubella syndrome (CRS). In addition to receiving supportive treatment, the patient was sent abroad for cataract excision and decongestive therapy for Patent ductus arteriosus (PDA).
Cases of this kind may recur because the nation lacks the Measles, Mumps, and Rubella (MMR) vaccine and a sufficient vaccination policy.
The infant patient’s mother did not have any prenatal screening during her pregnancy, which highlights the importance of providing healthy orientation to all expectant mothers in order to either prevent or address the illness.
Childbearing-age mothers should get the recommended vaccinations against rubella to prevent congenital rubella syndrome.
At-risk individuals should receive the MMR vaccine to prevent Congenital rubella syndrome and its complications.
Establishing and maintaining health surveillance systems is one of the other preventive and control measures.
Until an infant with Congenital rubella syndrome (CRS) is determined to be no longer contagious, health officials need to think about keeping them out of childcare centers.
It is important to inform parents and caregivers about the risk of their infants being exposed to pregnant individuals.
People who have contact with infants who have Congenital rubella syndrome (CRS) should possess official confirmation of their rubella immunity.
Effective prenatal care, as well as providing the MMR vaccine to all children and those who are at risk, can significantly contribute to the prevention and eventual elimination of the disease.
Conclusion
A term male baby born to an unvaccinated mother had sensorineural hearing loss, patent ductus arteriosus, bilateral congenital cataract, and other symptoms suggestive of congenital rubella syndrome.
This case highlights how urgently all women of childbearing age in our nation need to get the Measles, Mumps and Rubella (MMR) vaccine, and all pregnant women must receive appropriate prenatal care.
Ethical Approval
A case report is described in the article. Consequently, no further approval from our Ethics Committee was necessary.
Consent
Parental informed consent was obtained and happily satisfied for the release of the case facts, including the images that were taken.
Funding
We certify that no institution has provided funding for the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. https://www.mayoclinic.org/diseases-conditions/rubella/symptoms-causes/syc-20377310.
2. Seetoo K, Carlos MP, Blythe D, et al. Three cases of congenital rubella syndrome in the postelimination era. Maryland, Alabama, and Illinois. MMWR. Morbidity and Mortality Weekly Report. 2012;62(12):226.
3. 2019; Available from: https://www.who.int/news-room/factsheets/detail/rubella.
4. Givens KT, Lee DA, Jones T, Ilstrup DM. Congenital rubella syndrome: ophthalmic manifestations and associated systemic disorders. Br J Ophthalmol, 77 6 358–363 doi: 10.1136/bjo.77.6.358.
5. 2017; Available from: https://emedicine.medscape.com/article/968523-overview.
6. Numazaki K, Fujikawa T. Fujikawa T; Intracranial calcification with congenital rubella syndrome in a mother with serologic immunity.J Child Neurol. Journal of Child Neurology. 2003;18(4):296–297. doi:10.1177/08830738030180040601
7. Fang J, Agrawal A, Gowtham S, et al. Case Report: congenital rubella syndrome: a rare but persistent concern in the United States. J Perinatol. 2013;33(11):899–902. doi:10.1038/jp.2013.73
8. Seetoo K, Carlos MP, Blythe D, et al. Three cases of congenital rubella syndrome in the postelimination era—Maryland, Alabama, and Illinois. Morbidity and Mortality Weekly Report. 2012;62(12):226.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.