Back to Journals » Drug Design, Development and Therapy » Volume 18
Effect of Alleviating Preoperative Anxiety on Gastrointestinal Function Recovery After Laparoscopic High Ligation of the Hernia Sac in Children with Indirect Inguinal Hernia
Authors Chen X, Zhang X, Gao R, Huang Y, Mao S, Wang B, Feng J
Received 19 March 2024
Accepted for publication 29 July 2024
Published 5 August 2024 Volume 2024:18 Pages 3477—3486
DOI https://doi.org/10.2147/DDDT.S461097
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Georgios Panos
Xinyue Chen,1 Xue Zhang,2 Ruijia Gao,2 Yu Huang,3 Shimeng Mao,2 Bing Wang,4 Jiying Feng4
1Department of Anesthesiology, Jinzhou Medical University, Jinzhou, Liaoning, People’s Republic of China; 2Department of Anesthesiology, Xuzhou Medical University, Xuzhou, Jiangsu, People’s Republic of China; 3Department of Anesthesiology, Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China; 4Department of anesthesiology, the Affiliated Lianyungang Hospital of Xuzhou Medical University, the First People’s Hospital of Lianyungang, Lianyungang, Jiangsu, People’s Republic of China
Correspondence: Jiying Feng, No. 6 East Zhenhua Road, The Affiliated Lianyungang Hospital of Xuzhou Medical University, Lianyungang, Jiangsu, People’s Republic of China, Email [email protected]
Purpose: Anxiety and depression can affect the physiology of the gastrointestinal tract through the brain-gut axis, causing gastrointestinal dysfunction, which is mainly manifested as indigestion, diarrhoea, constipation, or abdominal pain. Preoperative anxiety arises in children due to separation from parents, fear of unfamiliar surroundings and anaesthesia and surgical procedures.To discuss the effect of alleviating preoperative anxiety on postoperative recovery of gastrointestinal function in children with indirect inguinal hernia after laparoscopic high ligation of the hernia sac.
Patients and Methods: 90 children with laparoscopic high ligation of the herniated sac in oblique inguinal hernia were randomly divided into control group (Group C) and experimental group (Group M). The Group M was given midazolam oral solution 0.5mg/kg (maximum dose 20mg), and The Group C was given 5% glucose solution with the same dose.Primary outcome was the time to first postoperative defecation and I-FEED scores.The secondary outcomes included mYPAS-SF scores; child sedation scores; child-parent separation scores; parental STAI scores;PHBQ scores;FLACC scores, operative time, and fluid input and surgeon job satisfaction.
Results: Compared with Group C, there was a shorter time to first postoperative defecation (P < 0.05), and lower I-FEED scores on postoperative day 1 (P < 0.05). The mYPAS-SF scores, which were significantly different in Group M at T1, T2, and T3 (P < 0.05), parental STAI scores at S1, child sedation scores and child-parent separation scores in T1, and surgeon job satisfaction between the two groups were significantly different (P < 0.05). There were no statistically significant differences in I-FEED scores on days 2 and 3, PHBQ scores, FLACC scores, operative time, and fluid input between the two groups of children (P > 0.05).
Conclusion: Preoperative application of midazolam oral solution to relieve preoperative anxiety helps to promote the recovery of postoperative gastrointestinal function in children with indirect inguinal hernia and increases the surgeon job satisfaction.
Keywords: preoperative anxiety, gastrointestinal function, midazolam:pediatric surgery
Introduction
Brain-gut axis is a collective term for the interconnecting pathways between the brain and the gut, which mainly include the autonomic nervous system, the hypothalamic-pituitary-adrenal axis, and the immune system. Research has found that preoperative anxiety delays the recovery of gastrointestinal function after surgery. Anxiety and depression can affect the physiology of the gastrointestinal tract through the brain-gut axis, causing gastrointestinal dysfunction, which is mainly manifested as indigestion, diarrhoea, constipation, or abdominal pain.1
Preoperative anxiety occurs in children due to separation from parents, fear of unfamiliar environments and anaesthesia and surgical procedures. Research findings have shown that preoperative anxiety is a relatively common phenomenon in preschool children, with approximately 65%-80% of children experiencing preoperative anxiety.2 Kain found many negative effects of preoperative anxiety, including prolonged induction of anaesthesia, poorer postoperative recovery, and higher postoperative analgesic dosage.3
Midazolam oral solution is the first oral benzodiazepine solution approved in China with indication for preoperative sedation in children. It has sedative-hypnotic, anxiolytic, anticonvulsant, myorelaxant, and anterograde amnesic effects, exerting the anxiolytic mechanism mainly through GABA receptors. It also has the advantages of good adherence, safety and controllability, and ease of use. It is used to relieve anxiety before surgery in children.4,5
The concept of enhanced recovery after surgery (ERAS) aims to reduce the physiological and psychological traumatic stress of surgical patients, minimise their functional damage, and promote their functional recovery by optimising the perioperative patient management measures, so as to achieve the goal of rapid recovery. Accelerating the recovery of postoperative gastrointestinal function is one of the important problems in the field of surgery nowadays, and it is also an important part of ERAS. To our knowledge, no study has examined the effect of preoperative anxiety and postoperative gastrointestinal recovery in paediatric patients. To fill this knowledge gap, we investigated the effect of alleviating preoperative anxiety via premedication with midazolam on postoperative gastrointestinal function recovery in paediatric patients undergoing laparoscopic high ligation of indirect inguinal hernia.
Materials and Methods
Participants
The study followed the relevant provisions of the Declaration of Helsinki by the World Medical Association and was approved by the Ethics Committee of the First People’s Hospital of Lianyungang on 10 February 2023 (KY-20221123001-01). The trial was registered at the Chinese Clinical Trial Registry (ChiCTR2300071196; date of registration: 8 May 2023).Single-centre study performed between April 4th 2023 and December 1st 2023. A total of 100 paediatric patients were enrolled in the study, out of which 10 paediatric patients were excluded. Finally, 90 paediatric patients were included in the analysis, 45 in Group M and 45 in Group C. We included children aged 2 to 6 years, with the American Society of Anesthesiologists physical status I–II, and who were scheduled for laparoscopic high ligation of indirect inguinal hernia. The exclusion criteria were the following: history of oral sedative-analgesic medication (benzodiazepines, barbiturates, non-steroidal anti-inflammatory drugs, opioid analgesics, etc). in the 14 days prior to surgery; diagnosed cognitive and developmental disorders; history of gastrointestinal dysfunction; history of prior surgeries; BMI of ≥ 25 kg/m2.
Preoperative Administration and Anesthesia
Written informed consent from the parents or guardians and verbal permission from the children were obtained. The children were taken to the pre-operative holding area (30 min before surgery) with one of their family members. Baseline anxiety levels (T0) were measured using the modified Yale Pre-operative Anxiety Scale-Short Form (mYPAS-SF).4 Then, the children were allocated to one of the two groups (Group M (midazolam) or Group C (5% dextrose solution)) using a sealed envelope technique. Midazolam (Humanwell Healthcare) 0.5 mg kg-1 was administrated orally to the children in Group M. Children in Group C were given an equivalent volume of 5% dextrose solution. Children stayed with one of their family members in the pre-operative holding area. At the same time, the baseline anxiety levels (S0) of parents were measured using Parental State-Trait Anxiety Inventory (STAI) scores. After out of the holding area (T1), children had their anxiety levels measured using mYPAS-SF. At once, sedation scores and parent-child separation scores were assessed. Then, they were transferred to the operating room unaccompanied, as per the policy of our hospital. The mYPAS-SF was assessed again while the children were entering the operating room (T2). After they were out of the holding area, parent’s anxiety levels were recorded using STAI scores (S1).
In the operating room, standard noninvasive monitoring was applied to all children. The mYPAS-SF was assessed during mask induction of anaesthesia (T3). Children were given general anesthesia with intravenous propofol (2–4 mg/kg), cis-atracurium (0.05–0.15 mg/kg), and sufentanil (0.1–0.3 ug/kg). Sevoflurane and remifentanil were given to maintain anesthesia. Sevoflurane was assessed with a minimal alveolar concentration (MAC) targeted at 1.0 (± 0.2) and remifentanil with 0.1–0.4 ug/(kg∙min). Children were ventilated with a 60% air-oxygen mixture and mechanically ventilated in PCV-VG mode (tidal volume, 8–10 mL/kg). The respiratory rate was regulated to 20–30 breaths/min and the partial pressure of end-tidal carbon dioxide was between 35 and 45 mmHg. After the end of surgery, all children were given 0.2% ropivacaine 1–3 mL for local closure of incisions. Then, they were awakened and transferred to the postanaesthesia care unit (PACU).
Children were observed for the time to first postoperative defecation and postoperative gastrointestinal function was assessed using the I-FEED score for 3 days. The PHBQ and FLACC scores were also observed for 3 days.
Observation Indicators
One of the investigators who was not directly involved in the care of the patient rated the study variables.
Modified Yale Pre-Operative Anxiety Scale-Short Form (mYPAS-SF) Scores
Anxiety was assessed using the mYPAS-SF score. This scale was simplified by Jenkins6 and has good reliability and validity. The mYPAS-SF score, which ranges from 23 to 100, is composed of 18 items distributed over four categories (activity, arousal, vocalisation, and emotional status). A score less than 24 indicates nonanxiety, a score from 24 to 30 indicates anxiety, and a score more than 30 indicates severe anxiety.
Intestinal Ischemia–Reperfusion Injury (I-FEED) Scores
I-FEED is a scoring system created by the American Society for Enhanced Recovery and Perioperative Quality. In 2018, a joint consensus statement published by the American Society for Enhanced Recovery and Perioperative Quality recommended the use of the I-FEED score to diagnose postoperative gastrointestinal dysfunction.7 In this form, patients are scored according to five items (intake, feeling nauseated, emesis, exam, and duration of symptoms). The scoring system attributes 0–3 points for each of the 5 components based on the clinical presentation of the patient and categorizes patients into normal (0–2), POGI (postoperative gastrointestinal intolerance: 3–5), and POGD (postoperative gastrointestinal dysfunction: ≥ 6). Studies have confirmed the validity of the I-FEED score in the assessment of postoperative gastrointestinal function.
Post Hospitalization Behavioral Questionnaire (PHBQ) Scores
The PHBQ is a questionnaire measuring post-hospitalization behavioral changes in children. The PHBQ has acceptable validity and reliability.8 The PHBQ consists of 27 items concerning sleep, eating, anxiety, aggressive behaviour, etc. For each item, the parent is asked to compare the child’s current (post-hospitalization) behaviour with the week before hospitalization. Five response alternatives are provided: “much less”, “less”, “unchanged”, “more”, and “much more” than before hospitalization. Each answer is given a score from 1 to 5. Total score is calculated by adding all responses. Factor analysis makes it possible to extract six subscales by grouping the items together. The subscales are general anxiety and regression, separation anxiety, anxiety about sleep, eating disturbance, aggression towards authority, and withdrawal.9
Face, Legs, Activity, Cry, Consolability (FLACC) Scores
The FLACC has been found to have reasonable inter-rater reliability and validity as a measure of pain in children with varying degrees.10 This simple tool contains five categories (Face, Legs, Activity, Cry, Consolability), each of which is scored from 0 to 2 to provide a total score ranging from 0 to 10.
Parent-Child Separation Scores
The parent-child separation score is used to assess the child’s sedation by the performance of sedated emotional parent-child separation.11 Unsuccessful separation is defined as a score of 1 or 2 on each item, and the child is unable to be removed from the guardian’s contact and sight. Successful separation is defined as a score of 3 or 4 for each item and the guardian is out of contact and sight of the child.
Sedation Scores
The scoring criteria are as follows: Grade I: sleepy, needs to be shaken and shouted to wake up, unresponsive when separated from parent; Grade II: asleep, eyes closed, can be woken up by soft voice or movement, no apparent resistance when separated from parent; Grade III: slightly asleep, can open eyes, but little activity, indifferent response when separated from parent; Grade IV: awake, calm, uncooperative when separated from parent; Grade V: Irritable, cries and struggles when separated from parents. Grades I to III are valid; Grades IV to V are invalid.
Statistical Analysis
Before beginning this study, we performed a pilot study to identify the sample size. According to the results of the pre-experiment, the mean value of time to first postoperative defecation in Group M was 10.23, and the standard deviation was 3.15. The mean value of time to first postoperative defecation in Group C was 13.69, and the standard deviation was 7.31. A total of 84 patients were required with a two-sided alpha of 5% and achieving 90% power (t-test). We anticipated 10% dropout, and considering the 1:1 ratio, 90 patients were eventually included in the study.
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 27.0. The normality of the quantitative variables was assessed using the Shapiro–Wilk test. Normally distributed data were presented as means and standard deviations. Homogeneity of variances was evaluated using Levene’s test. Normally distributed data with equal variances were analyzed using the independent samples t-test, while data with unequal variances were analyzed using Welch’s t-test. Skewed data were depicted using the median and interquartile range and were analyzed using the Mann–Whitney U-test. All tests were two-tailed, and statistical significance was defined as P < 0.05.
Results
A total of 100 patients were assessed, and 7 patients were excluded due to the cancellation of the surgery. A total of 93 patients entering the study were randomly allocated to two groups. 2 patients in Group M and 1 patient in Group C failed to complete the study. Finally, 45 patients in Group M and 45 patients in Group C were included in the analysis (Figure 1).
 |
Figure 1 Flowchart of patient selection. |
No difference between the two groups were observed in terms of demographic data and surgical characteristics (Table 1 and 2).
 |
Table 1 Demographic Data |
 |
Table 2 Surgical Characteristics |
The time to first postoperative defecation and I-FEED scores are shown in Table 3. The time to first postoperative defecation in Group M is lower than that in Group C (P < 0.001). The time to first flatus in Group M was 7.1 (5.1,8.5), lower than that in Group C 10.8 (8.7,20.0). The defecation time in Group M was 8.1 (6.8,10.6), lower than that in Group C 12.1 (8.9,21.6). The main effect of the I-FEED score was different between the two groups on day 1(P = 0.006). The I-FEED score was lower on day 1 in Group M. The I-FEED score in Group M was 0.0 (0.0,0.0), lower than that in Group C 0.0 (0.0,1.0).
 |
Table 3 Time to First Postoperative Ventilation and Defecation and I-FEED Scores |
Table 4 shows the comparison of mYPAS-SF scores at each time point. There was no difference in the baseline (T0) mYPAS-SF scores between two groups (P = 0.180). The mYPAS-SF scores were significantly different between the groups at T1, T2, and T3 (P < 0.001, respectively). Specifically, the mYPAS-SF score at T1 was 22.9 (22.9,27.1), lower in Group M than in Group C (72.9 (56.3,90.6)). The mYPAS-SF score at T2 was 22.9 (22.9,27.1), lower in Group M than that in Group C (72.9 (56.3,95.8)). The mYPAS-SF score at T3 was 22.9 (22.9,27.1), lower in Group M than that in Group C (79.2 (68.9,95.8)). When we classified the mYPAS-SF score more than 23 as anxiety, the prevalence of anxiety was different between the groups at T1, T2, and T3 (P < 0.001, respectively, Figure 2).
 |
Table 4 Modified Yale Preoperative Anxiety Score-Short Form |
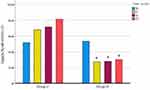 |
Figure 2 The mYPAS-SF score more than 23 as anxiety, the prevalence of anxiety was different between the groups at T1, T2, and T3 *P < 0.001, respectively. |
There were significant differences between the groups at sedation scores and parent-child separation scores in Table 5 (P < 0.001, respectively). Sedation scores in Group M were (3 (3,3)), lower than that in Group C 4 (4,5). Parent-child separation scores in Group C were 6 (3,7), lower than that in Group M (9 (9,9)).
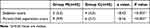 |
Table 5 Sedation Score and Parent-Child Separation Score |
Table 6 shows the comparison of Parental STAI scores at each time point. There was no difference in STAI scores at the baseline (S0) between two groups (P = 0.067). The STAI scores were significantly different between the groups at S1 (P = 0.025). The score at S1 was 79.0±7.9 in Group M, lower than that in Group C (82.8±8.0).
 |
Table 6 Parents STAI Score |
Table 7 shows the percentage comparison of surgeon job satisfaction between two groups. There was a significant difference between the two groups (P = 0.001). The overall satisfaction rate in Group M was 91.1%, higher than that in Group C (82.2%). There was no statistically significant difference in PHBQ scores, FLACC scores, operative time and infusion volume.
 |
Table 7 Surgeon Job Satisfaction |
Discussion
In the present study, we investigated the effect of preoperative anxiety on postoperative recovery of gastrointestinal function in paediatric patients. We found that alleviating preoperative anxiety via premedication with midazolam helps to promote the recovery of postoperative gastrointestinal function in paediatric patients after laparoscopic high ligation of inguinal hernia sac.
With the development and advancement of medical technology, the status of rapid perioperative recovery of patients has received more and more attention. The concept of ERAS is to promote the rapid recovery of patients by reducing the patient’s stress caused by surgical trauma and other management measures. Accelerated recovery of postoperative gastrointestinal function is an important part of ERAS components and an area of increasing interest for surgeons and even anaesthesiologists. In a study evaluating the reliability, safety, efficacy, and cost of ERAS programmes in a population of children undergoing gastrointestinal surgery, it was stated that ERAS programmes are safe and feasible for children undergoing gastrointestinal surgery, guaranteeing economic benefits, improving patient recovery, shortening hospital stays, accelerating gastrointestinal recovery, and reducing perioperative fluids and postoperative opioid use for pain relief.12
Research has found that preoperative anxiety delays recovery of postoperative gastrointestinal function. Negative emotions such as anxiety and depression cause activation of the hypothalamic-pituitary-adrenal axis (HPA) and an increased stress response in humans, which in turn causes the increase of cortisol and adrenaline levels and triggers natural killer cell activity. These changes delay wound healing and suppress the immune system, thereby increasing susceptibility to infections and tumour diseases.1 In addition, psychological stress may lead to gut microbiota translocation, with stress decreasing specific intestinal epithelial tight junction proteins and compromising the integrity of the intestinal epithelium, thereby altering intestinal motility, affecting secretion and mucin production, and ultimately leading to alterations in microbial composition and intestinal permeability.13 Kim et al found that the application of buspirone to mice significantly suppressed stress-induced anxiety- or depression-like behaviours, and altered the composition of the intestinal microbiota in mice.14 As for clinical research, Liu Yuqi et al’s study on patients undergoing gynaecological laparoscopic surgery found that negative emotions such as nervousness and anxiety can affect the time to first flatus, and that the level of anxiety may be one of the predictive indicators of longer time to first flatus.15
In our studies, the time to first postoperative flatus and defecation was shorter in Group M than in Group C, and the I-FEED score was lower on the first postoperative day, suggesting that alleviation of preoperative anxiety can promote recovery of gastrointestinal function in the postoperative period. The I-FEED scores on day 1 were not diagnostic of postoperative gastrointestinal disturbances in either group (≥ 6). There was no difference in I-FEED scores between the two groups on postoperative days 2 and 3, and it was considered that this might be due to the brevity of the procedure chosen for this study, and further studies will be conducted in the future.
Preoperative anxiety is more severe in children due to their cognitive limitations, resulting in fear, crying, dread, difficulty separating from parents and even avoidance. Five factors are found to have a significant effect on children’s anxiety: age, parental anxiety, previous hospitalisation history, socialization, and surgical environment.16 Children with preoperative anxiety disorders are three times more likely to experience confusion, nightmares, separation anxiety, sleep disturbances, nighttime crying, enuresis, temper tantrums, apathy, withdrawal, eating disorders, and negative behavioural changes than non-anxious individuals.17,18 These negative behaviours can be observed even a year after discharge, which can have a long-term negative impact on children’s future medical interactions and impede their normal growth and development. Therefore, interventions to alleviate preoperative anxiety are clinically important.
In this study, the children in the test group had lower mYPAS-SF scores at T1, T2, and T3, as well as lower sedation scores and parent-child separation scores, indicating that midazolam oral solution has a good anxiolytic effect.
However, there was no significant difference in PHBQ score and FLACC score between the two groups in this study. It may be because 1) the high ligation of the hernia sac is a short operation with small wound and quick recovery; 2) The observed postoperative time range was short, and no long-term postoperative follow-up was conducted. Further studies will be conducted in the future.
Traditional open indirect inguinal hernia surgery is traumatic and slow to recover. With the continuous development of laparoscopic technology, laparoscopic hernia surgery can make up for the shortcomings of traditional open surgery and achieve better treatment results. However, laparoscopic surgery is more of a test of the clinician’s technical level, who can observe less of the abdominal cavity. The operation is difficult and can be affected by a variety of factors. Children who cry and swallow too much gas become bloated, which makes the operating space narrower and more difficult for the surgeon to operate. In our study, surgeons in Group M were more satisfied with intraoperative operations compared to Group C. In terms of pain scores and postoperative behavioural recovery scores, there was no difference between the two groups, which may be due to the fact that firstly, most of the current paediatric hernia surgeries are performed laparoscopically, which has a small incision, less pain, faster recovery, and fewer complications, and all the patients took analgesia at the wound site. Secondly, the postoperative behavioural recovery may require a long period of observation, and the present study was not able to explore the long-term negative impacts of anxiety due to limited conditions.
In addition, parental anxiety can have a negative impact on children. A study by Getahun et al found that parental anxiety levels in the preoperative holding area were positively correlated with children’s perioperative anxiety levels, and that parental anxiety led to a 3.43-fold increase in the incidence of anxiety in children in the operating room.15,19 Parents can experience increased anxiety when their children struggle with separation anxiety while leaving the holding area, due to their high dependence on their parents. In this trial, parents’ anxiety levels were significantly lower when children left the holding area (S1) in Group M than in Group C, suggesting that alleviating children’s anxiety may also alleviate parents’ anxiety. In the future, interventions that reduce parental anxiety and help them cope with it appropriately may be more important than reducing child anxiety alone.20,21 These may include providing parents with information about anaesthetic procedures, enabling them to communicate with doctors and other parents in similar situations, giving them emotional support, and guiding them to help their children more effectively.
Conclusion
The preoperative application of midazolam oral solution to relieve preoperative anxiety can help to promote the recovery of postoperative gastrointestinal function in children undergoing laparoscopic high ligation of indirect inguinal hernia, and increase the surgeon job satisfaction.
Registration Statement
Our clinical trial was registered via phone prior to patient enrolment, with subsequent online registration once it was possible. The date of our phone registration was March 28, 2023, the date of our online registration was May 8, 2023 and the date of first patient enrolment was April 4, 2023.
Data Sharing Statement
The data sets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
We thank the participants and clinic staff for their contributions to the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vaga S, Lee S, Ji B. et al. Compositional and functional differences of the mucosal microbiota along the intestine of healthy individuals. Scientific Reports. 2020;10(1). doi:10.1038/s41598-020-71939-2
2. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiologica. 2018;84(11). doi:10.23736/S0375-9393.18.12520-X
3. Kain ZN, Mayes LC, Caldwell-Andrews AA, et al. Preoperative Anxiety, Postoperative Pain, and Behavioral Recovery in Young Children Undergoing Surgery. Pediatrics. 2006;118(2):651–658. doi:10.1542/peds.2005-2920
4. Xiong H, Liu J, Liu G, et al. Effective doses of midazolam oral solution for the prevention of preoperative anxiety in paediatric patients. international Journal of Paediatric Dentistry. 2024. doi:10.1111/ipd.13162
5. Manso MA, Guittet C, Vandenhende F, Granier LA. Efficacy of oral midazolam for minimal and moderate sedation in pediatric patients: a systematic review. Paediatr Anaesth. 2019;29(11):1094–1106. doi:10.1111/pan.13747.
6. Jenkins BN, Fortier MA, Kaplan SH, Mayes LC, Kain ZN. Development of a Short Version of the Modified Yale Preoperative Anxiety Scale. Anesthesia & Analgesia. 2014;119(3):643–650. doi:10.1213/ANE.0000000000000350
7. L HT, D MM, G MMM, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Postoperative Gastrointestinal Dysfunction Within an Enhanced Recovery Pathway for Elective Colorectal Surgery. Anesthesia & Analgesia. 2018;126(6):1896–1907. doi:10.1213/ANE.0000000000002742
8. Banchs RJ, Lerman J. Preoperative Anxiety Management, Emergence Delirium, and Postoperative Behavior. Anesthesiology Clinics. 2014;32(1):1–23. doi:10.1016/j.anclin.2013.10.011
9. Karling M, Stenlund H, Hägglöf B. Behavioural changes after anaesthesia: validity and liability of the Post Hospitalization Behavior Questionnaire in a Swedish paediatric population. Acta Paediatrica. 2006;95(3):340–346. doi:10.1080/08035250500434751
10. Malviya S, Lewis VOEPEL, Burke T, et al. The revised FLACC observational pain tool: improved reliability and validity for pain assessment in children with cognitive impairment. Pediatric Anesthesia. 2006;16(3):258–265. doi:10.1111/j.1460-9592.2005.01773.x
11. Navarro-Tapia E, Almeida-Toledano L, Sebastiani G, et al. Effects of Microbiota Imbalance in Anxiety and Eating Disorders: probiotics as Novel Therapeutic Approaches. International Journal of Molecular Sciences. 2021;22(5):2351. doi:10.3390/ijms22052351
12. Arena S, Di Fabrizio D, Impellizzeri P, et al. Enhanced Recovery After Gastrointestinal Surgery (ERAS) in Pediatric Patients: a Systematic Review and Meta-analysis. Journal of Gastrointestinal Surgery. 2021;25(11):2976–2988. doi:10.1007/s11605-021-05053-7
13. Kim J, Han S, Joo M, et al. Buspirone alleviates anxiety, depression, and colitis; and modulates gut microbiota in mice. Scientific Reports. 2021;11(1):
14. Yuqi LIU, Qingyan LUO, Shaoqiang HUANG, et al. Effect of anxiety and depression status on postoperative pain in gynaecological laparoscopic surgery patients. Journal of Clinical Anaesthesiology. 2018;34(03):254–257.
15. Liu W, Xu R, E JJ, et al. Research Progress on Risk Factors of Preoperative Anxiety in Children: a Scoping Review. International Journal of Environmental Research and Public Health. 2022;19(16):9828. doi:10.3390/ijerph19169828
16. Risk factors associated with anesthesia emergence delirium in children undergoing outpatient surgery. Br-Azilian Journal of Anesthesiology. 2018;68(2):162–167. doi:10.1016/j.bjane.2017.11.002
17. Aykut A, Işik B. Emotion regulation and premedication success relationship in children whose underwent general anesthesia. TURKISH JOURNAL of MEDICAL SCIENCES. 2018;48(2). doi:10.3906/sag-1702-117
18. Gooden R, Tennant I, James B, et al. The incidence of emergence delirium and risk factors following sevoflurane use in pediatric patients for day case surgery, Kingston, Jamaica. Brazilian Journal of Anesthesiology. 2014;64(6):413–418. doi:10.1016/j.bjane.2013.09.012
19. Djupesland PG, Messina JC, Mahmoud RA. Magnitude and Factors Associated with Preoperative Anxiety Among Pediatric Patients: cross-Sectional Study. Therapeutic Delivery. 2020;Volume 11(8):485–494. doi:10.2147/PHMT.S288077
20. Cagiran E, Sergin D, N DM, et al. Effects of sociodemographic factors and maternal anxiety on preoperative anxiety in children. Journal of International Medical Research. 2014;42(2):572–580. doi:10.1177/0300060513503758
21. Cui X, Zhu B, Zhao J, et al. Parental state anxiety correlates with preoperative anxiety in Chinese preschool children. Journal of Paediatrics and Child Health. 2016;52(6):649–655. doi:10.1111/jpc.13176
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
