Back to Journals » Risk Management and Healthcare Policy » Volume 17
Enhancing Standardized Practices for Oral Mucositis Prevention in Pediatric Hematopoietic Stem Cell Transplantation: A Best Practice Implementation Project
Authors Zhang L, Luo Y, Long J, Yin Y , Fu Q, Wang L, Patil S
Received 2 April 2024
Accepted for publication 31 July 2024
Published 6 August 2024 Volume 2024:17 Pages 1909—1920
DOI https://doi.org/10.2147/RMHP.S471877
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Luyang Zhang,1,* Yuan Luo,1,* Jiewen Long,1 Yan Yin,1 Qin Fu,2 Lei Wang,1 Sandip Patil1
1Department of Haematology and Oncology, Shenzhen Children’s Hospital, Shenzhen, Guangdong Province, People’s Republic of China; 2Department of Nursing, Shenzhen Children’s Hospital, Shenzhen, Guangdong Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Sandip Patil; Lei Wang, Department of Haematology and Oncology, Shenzhen Children’s Hospital, 7019 Yitian Road, Shenzhen, Guangdong Province, People’s Republic of China, Tel +86-755-83008283, Email [email protected]; [email protected]
Background: Oral mucositis (OM) poses a significant challenge in children undergoing hematopoietic stem cell transplantation (HSCT). There is a gap between clinical practice and the evidence, and nursing practices is not standardized.
Objective: This study aims to evaluate the effectiveness of applying the evidence for preventing HSCT chemotherapy-induced OM in children and to elevate the nurses’ compliance to the evidence.
Methods: Following the clinical evidence practice application model of the Joanna Briggs Institute (JBI) evidence-Based Care Center. The process included reviewing literature, extracting evidence, identifying gaps, developing audit criteria, conducting a baseline audit, creating an action plan, implementing evidence-based interventions, and assessing outcomes.
Results: After the evidence implementation, 6 out of 12 audit criteria with poor compliance are significantly improved, with statistically significant differences (P< 0.05). The incidence of OM decreases, with a statistically significant difference (66.6% vs 36.7%, P=0.02). The incidence of grade I, II, III, and IV OM also decreases (30% vs 23.3%, 23.3% vs 13.4%, 10% vs 0%, and 3.3% vs 0%). Ultimately, the standardized oral care practice routine and workflows to prevent OM were established.
Conclusion: Bridging the gap between evidence and clinical practice can standardize nurse behavior, decrease the incidence of OM, and lower the OM severity in children undergoing HSCT.
Keywords: children, hematopoietic stem cell transplantation, oral mucositis, evidence-based practice
Background
Oral mucositis (OM) refers to the pathological changes in oral mucosal caused by cytotoxic effects of chemotherapy,1 which is recognized as one of the most frequent complications of chemotherapy.2 Hematopoietic stem cell transplantation (HSCT) emerges as the most potent cure for several malignant and nonmalignant diseases.3 However, it generally is leads to OM, as 43–97% of pediatric patients who underwent HSCT are reported to suffer from OM.4–7 OM typically manifests early in the course of HSCT treatment, peaking around 7–14 days post-conditioning regimen initiation, often accompanied by painful ulcers.8 The clinical presentation of OM includes erythema and ulcerations with varying degrees of intensity.9 In addition, OM can increase care costs, aggravate pain, severe nutritional deficiencies, and malnutrition, reduce the chemotherapy dose or even treatment interruptions, and prolong the hospitalization.10–13 Therefore, effective preventive strategies are imperative to prevent burden of OM in HSCT pediatric patients.
The best evidence for managing OM in pediatric HSCT patients primarily includes cryotherapy with high-dose melphalan or 5-fluorouracil, photobiomodulation, and avoiding routine administration of palifermin and granulocyte colony-stimulating factor (GCSF) for OM prevention, et.14 However, current clinical practice often relies heavily on empirical approaches rather than standardized practice. There is a gap between clinical practice and the evidence. Furthermore, children face unique challenges such as increased difficulty in adhering to preventive measures compliance, which further complicates the management of OM in this vulnerable group.
Nurses play a critical role in intervening OM. However, integrating evidence into practice poses challenges. In clinical settings, evidence-based medicine refers to “the conscientious, explicit, and judicious use of the current best evidence in making decisions about the care of individual patients”.15 Additionally, clinical practice is also based on experience and routine influence clinical decision-making besides the evidence. A cross-sectional study that included 157 nurses on oncology nursing practices for managing chemotherapy-induced OM according to evidence-based guidelines reveals the deficiencies in implementing written OM protocols and guidelines.16 Meanwhile, nurses’ internal factors, including knowledge, attitudes, and skills about the evidence-based practice, as well as their personal readiness or preparation for implementing evidence-based practice can affect its implementation.17 Furthermore, organizational barriers (such as workload, staff/management showing no support for evidence based practice, insufficient resources, the lack of authority to change practice, and a workplace culture resistant to change) would impact an individual’s ability to increase and maintain the evidence-based practice.18 Therefore, applying the evidence is essential to prevent OM in HSCT pediatric patients to reduce the incidence of OM, mitigate its severity, and increase nurses’ compliance with the evidence.
Data and Methods
Summary of Evidence
Problem Establishment
The research question was constructed based on the clinical questions. The PIPOST model structure from the Fudan University Evidence-Based Nursing Research Center was employed for search. The PIPOST can be explained as follows: P (population): children undergoing HSCT; I (intervention): basic oral care, dental examination, oral cryotherapy, and health education; P (professional): nurses and caregivers; O (outcome): (1) incidence of OM; (2) severity of OM; (3) nurses’ compliance with the implementation of audit criteria for OM; S (setting): pediatric HSCT center; T (type): clinical practice guidelines, evidence summary, systematic review, and expert consensus.
Evidence Retrieval
A systematic search was conducted using the 6S Hierarchy of evidence model in a top-down approach to ensure the inclusion of the most relevant and high-quality studies.19 The key terms for the search were determined based on the Mesh subject headings and keywords identified in the pre-search literature. These keywords included “pediatric”, “child*”, “oral mucositis”, “stomatitis”, “hematopoietic stem cell transplantation”, “HSCT”, “chemotherapy”, “neoplasms”, and “cancer”, “clinical decision” or guideline or “evidence summary” or “systematic review”. The search was conducted on the British Medical Journal (BMJ) Best Practice, UpToDate, the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO), the JBI evidence-Based Database, the Cochrane Library, as well as the websites of the Registered Nurses Association of Ontario (RNAO), the Scottish Intercollegiate Guidelines Network (SIGN), and National Institute for Health and Care Excellence (NICE). The searched literature should be published from January 1, 2018, to December 31, 2022. The literature search process is depicted in Figure 1.
 |
Figure 1 Flow Chart of the Literature Search Process. |
Basic Information and Quality Assessment Results of Included Literature
Inclusion and Exclusion Criteria for Literature
Inclusion criteria: (1) Articles focusing on the management and prevention of OM in children undergoing HSCT; (2) Types of evidence: clinical practice guidelines, evidence summaries, systematic reviews, and expert consensus; (3) Language: English; and (4) Duration: from January 1, 2018, to December 31, 2022. Exclusion criteria: Studies mentioning adult patients; guideline interpretations; abstracts; research proposals; and documents that were not accessible in full text or were duplicated and directly translated. Ultimately, 2 evidence summaries20,21 and 1 guideline14 were included for analysis in this research.
Quality Assessment of Literature
The quality of the guidelines was assessed using the AGREE II instrument,22 and the quality evaluation of the evidence summary entails tracing back to the original literature that underpins the evidence, and selecting suitable evaluation tools for quality assessment based on the type of research. Two members engaging in evidence-based nursing read and extracted the required information from the included literature independently. Any conflicting assessment opinions between them can be arbitrated by a third researcher.
Evidence Translated into Clinical Audit Criteria
Based on the JBI Grades of Recommendation,23 Grade A recommendations were strongly supported by evidence for implementation, while Grade B recommendations exhibited weak evidence support for consideration. Through feasibility, appropriateness, meaningfulness, effectiveness (FAME) argumentation,23 evidences were translated into clinical audit criteria.
Evidence Implementation
The clinical setting for this research was the HSCT center of a tertiary children’s hospital in Shenzhen, with 26 laminar flow cabinets and a total of 33 nurses. Nurses at the HSCT center and children undergoing HSCT were selected as the subjects for audit before and after implementing the evidences. Inclusion criteria for children: (1) Those who will undergo HSCT; (2) Children determined as grade 0 (no mucosal change) according to the World Health Organization (WHO) OM grading criteria24 before conditioning; and (3) Informed consent was obtained from their guardians prior to their inclusion in the study. Exclusion criteria for children: (1) Children with cognitive impairment; (2) Children experiencing previous radiation therapy before chemotherapy; and (3) Those with pre-chemotherapy conditions like OM (graded I to IV according to the OM grading criteria of the WHO), cavities, or periodontal diseases. Inclusion criteria for nurses: (1) Registered nurses working in the transplantation center. Exclusion criteria for nurses: (1) Nurse trainees. This work followed the JBI framework for evidence implementation and was performed based on the JBI’s online tools, such as Practical Application of Clinical evidence System (PACES) and Getting Research into Practice (GRIP) for reviews from May to July 2023.
Formation of the Evidence Implementation Project Team
An evidence implementation project team comprising six individuals was established, featuring distinct yet complementary roles: a Head Nurse, two team leaders, two specialty nurses, and a Chief Physician. Collectively, the team undertakes responsibilities in overall guidance, technical support, resource allocation, coordination, quality control, evidence searching, project design, educational training, data analysis, report writing, clinical supervision, data collection, personnel communication, and project promotion. This integrative structure guarantees comprehensive oversight and efficient execution of the project.
Outcome Evaluation
Incidence of OM
Oral assessments were conducted twice daily by the charge nurses utilizing the WHO tool. Furthermore, assessments were promptly carried out whenever patients reported any oral discomfort. The incidence and severity of oral OM were evaluated and calculated as part of the study outcomes.
- Incidence of OM: calculated as a percentage.
- Severity of OM: calculated as the percentage incidence of OM in Grades I to IV. The severity of OM was determined based on the OM grading standards issued by WHO. Grade 0: no mucosal change; Grade I: erythema and soreness; Grade II: erythema and ulcers, but the patient can swallow solid food; Grade III: ulcers, extensive erythema, patient cannot swallow solid food; Grade IV: severe mucositis with no possible alimentation.24
Audit Criteria
The compliance rate of the 12 audit criteria was recorded by marking “yes (Y)” for compliance and “no (N)” for non-compliance. The compliance rate was calculated using the number of compliant cases or times / total cases or times × 100%. Subsequently, the data were introduced into the computer system and the compliance rate for each audit criterion was calculated.
Statistical Methods
Data were statistically analyzed using SPSS version 26.0. Categorical data were described using case numbers and percentages, while continuous data were described with mean ± standard deviation. Continuous and categorical variables were analyzed utilizing Fisher’s exact test, with P<0.05 indicating statistical significance.
Results
Establishment of Audit Criteria and Review Methods
Based on the 8 evidences identified, the evidence Implementation Project Team has formulated twelve audit criteria. These evidences, together with the respective criteria and data collection methods for each, are detailed in Table 1.
 |
Table 1 Evidence and Audit Criteria for the Prevention of Chemotherapy-Induced Oral Mucositis in Pediatric HSCT Patients |
Baseline Audit
The evidence-Based Audit Criteria for Preventing OM in Children Undergoing HSCT Chemotherapy was developed based on the evidences obtained. Clinical nurses recorded whether each audit criterion was implemented through on-site review, medical record examination, video surveillance, on-site interviews with caregivers etc., as shown in Table 1. Using the PACES method, the baseline audit was conducted from May to July 2023, with a total of 30 patient cases reviewed, including 17 males (56.7%) and 13 females (43.3%), as outlined in Table 2.
 |
Table 2 Patient Characteristics |
Evidence Implementation
The baseline audit revealed that the implementation of C2.1, C2.2, C3.1, C4.1, C5, and C6 was suboptimal. To address this, the i-PARIHS evidence-based practice conceptual framework25 was employed to analyze facilitating factors and barriers to generate an action plan. Evidence was applied from October to December 2023, with a total of 30 patient cases reviewed, including 23 males (76.7%) and 7 females (23.3%), as outlined in Table 2
Facilitating Factors and Barriers
The facilitating factors and barriers impacting the implementation of evidence-based practices for the prevention of chemotherapy-induced oral mucositis (OM) in children undergoing hematopoietic stem cell transplantation (HSCT) were identified, as shown in Table 3. Key factors and challenges were assessed across the dimensions of innovation, recipients, and organizational level. Based on these assessments, an action plan was developed, focusing on these dimensions, as illustrated in Table 4.
 |
Table 3 Facilitating Factors and Barriers |
 |
Table 4 Action Plan for Audit Criteria C2.1, C2.2, C3.1, C4.1, C5, C6 |
Improvement of System Processes
The OM care routines were revised based on evidence, enabling the development of toothbrush management schemes and standardized workflow for oral cryotherapy. The educational implementation plan was enhanced with two versions: for caregiver education and for child education.
OM Incidence
Compared with the baseline group, the OM incidence decreased from 66.6% to 36.7% (X2=5.4, P=0.02) in the implementation group, showing statistical significance. Furthermore, the incidence of OM in Grades I, II, III, and IV decreased, with 30% vs 23.3%, 23.3% vs 13.4%, 10% vs 0%, and 3.3% vs 0%, respectively, as outlined in Table 5.
 |
Table 5 Comparison of OM Incidence |
Nurse Compliance Before and After Evidence Implementation
In contrast to the baseline group, nurse compliance in C2.1, C2.2, C3.1, C4.1, C5, and C6 was significantly improved, with the values of 0% vs 86.7%, 0% vs 86.7%, 33.3% vs 86.7%, 0% vs 100%, 6.7% vs 97.3%, and 6.7% vs 84.8%, respectively, showing statistical significances (P<0.001). The overall compliance rates of clinical nurses with the 12 audit criteria are summarized and compared in Table 6.
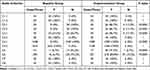 |
Table 6 Comparison of Compliance with Audit Criteria Before and After Evidence Implementation |
Discussion
Before implementing the evidence, our center identified a gap between the clinical practices for preventing OM and the available evidence and realized that bridging this gap is crucial for facilitating the successful translation of evidence into clinical outcomes.26 Moreover, it is imperative to formulate audit criteria based on the evidence in clinical practice and to promote the evidence-based clinical practices through changes and outcome evaluations, thus continuously improving the clinical quality.27 This work was commenced by identifying the problems, establishing teams, and systematically retrieving the evidences. Clinical evidence implementation necessitates thorough consideration of the evidence’s recommendation level and the clinical context due to its high significance.28 Unlike chemotherapy for typical pediatric oncology patients, children undergoing HSCT require high-dose chemotherapy and immunosuppressant agents for myeloablative conditioning regimen in laminar flow cabinets. Not all evidence related to radio and chemotherapy for pediatric patients is applicable to those undergoing HSCT due to the unique requirements of the HSCT process. For instance, maintaining a sterile environment within laminar flow rooms restricts the use of instruments and devices that cannot be adequately sterilized. Additionally, the immune system impairment resulting from HSCT necessitates minimizing the patient’s time outside the laminar flow cabin, thereby limiting access to certain examinations or treatments. Dietary restrictions for immunosuppressed patients also preclude the use of supportive treatments such as honey or sweet-sour candies, further limiting the applicability of general preventive measures for chemotherapy-induced oral mucositis (OM) in this specialized population. Consequently, we excluded evidence pertaining to photobiomodulation therapy and the use of honey. This underscores the necessity to explore the introduction of photobiomodulation therapy and the aseptic preparation of honey for clinical use, aiming to further reduce the incidence of OM. Consequently, it is essential to tailor interventions to the specific clinical context of these patients. Through a systematic literature review, this research incorporated the evidences associated with OM prevention in patients undergoing HSCT, translated the evidence into audit criteria, conducted a baseline audit, thoroughly analyzed the facilitating factors and barriers, and developed effective strategies for change implementation and outcome evaluation.
Furthermore, a baseline audit before evidence implementation showed that 6 audit criteria were either not initiated or implemented suboptimally. To enhance the nurses’ compliance to the audit criteria, it is crucial to effectively identify the facilitating factors and barriers, develop appropriate action plans, and actively secure resources. Identifying barriers plays a critical role in clinical translation of evidence across multiple evidence-based practice theoretical models.29 In this research, the i-PARIHS framework was employed to analyze the facilitating factor and barriers of the 6 audit criteria with poor compliance in terms of innovation, recipients, and context, aiming to formulate evidence-based practice action plans suited to our center.
Training in OM knowledge can enhance self-care and oral health compliance. In consideration of this, patients and caregivers are recommended to be trained with relevant knowledge of OM.30–32 Previous studies, though not specifically targeting HSCT patients, have indicated improvements in patient education and oral care practices,33–35 which align with the results of the current study. Nonetheless, those studies predominantly involved adult participants. In contrast, this research uniquely addresses pediatric patients, who encounter distinct and potentially more significant challenges in adhering to these oral care protocols. Before application of the evidence-based practice, nurses only educated caregivers on OM prevention, which was not comprehensive. Moreover, educating the children undergoing HSCT was neglected due to their young age, leading to low cooperation in oral care among some patients due to a lack of awareness of its importance. To address this, this research emphasized the importance of educating children, enhanced the education on children, and developed some age-appropriate health education methods (including animated videos, images, and models). In terms of brushing teeth, medical play was adopted to educate children, which could increase their engagement.
Moreover, this research refined the health education implementation scheme and segmented it into two parts: for the caregiver and for the children education, to comprehensively supervise the advancement of health education for children. Regarding oral care, all patients were required to use cotton swabs dipped in 0.9% saline solution for oral cleansing, which might not remove food residues between teeth. Given the toothbrush sterilization and the risk of gingival bleeding during low platelet counts as barriers, clinical implementation of tooth brushing was not practiced before applying evidence. During the change, the toothbrush sterilization was solved by supplementing necessary equipment and materials and providing sterilization cabinets. Meanwhile, toothbrush management schemes were established, including listing toothbrushes on patient supply preparation checklist, using sterilized soft-bristle toothbrushes changed daily, and implementing indicator C4.2 (applying solution with sterile gauze or using a suction tube) four times daily at platelet counts below 30*109/L. These strategies effectively solved the implementation barriers, so this standard has now become a routine part of oral care practices for our department. After HSCT, the salivary flow rate presents a decrease tendency, which can negatively impact saliva’s protective functions and potentially lead to oral complications.36
Low salivary flow rate has been identified as a risk factor for OM.37,38 However, clinical settings did not focus on the presence of dry mouth in patients before evidence implementation, lacking relevant regulations, resulting in a low compliance rate. In addition, oral cryotherapy exhibited its potential to reduce the incidence of OM in HSCT patients,39,40 but its clinical application was suboptimal, with nurses typically using it based on experience rather than a standardized workflow. In this research, specific regulations for assessing and intervening in cases of Xerostomia and a standardized workflow for oral cryotherapy based on the evidence were developed to facilitate better clinical evidence implementation.
Additionally, applying oral cryotherapy gives a precise requirement on timing, but nurses often fail to do it, increasing the challenging. Therefore, this research embedded oral cryotherapy into PDA system, with automatically pop-up reminders prior to the commencement of chemotherapy, thus advancing the evidence-based nursing practices. Cryotherapy typically involves holding ice chips in the mouth, which is a method with challenging to apply in children.39 An alternative approach using ice-cold 0.9% saline solution was considered, but maintaining the solution temperature during the oral cryotherapy is challenging. To address this, 500 mL of 0.9% saline solution was placed into a specialized freezing unit to turn it into ice and then thawed at room temperature four hours before use. These operations in this research could ensure that the solution is half-melted when administered to patients. Consequently, this method guarantees the maintenance of the temperature at ice water during oral cryotherapy and allows for continuous replenishment of the ice saline solution, thereby enhancing the intervention effectiveness.
Furthermore, it is essential to identify “local opinion leaders”,41 as they possess informal influence and their opinions and actions are readily accepted and followed by others. Thus, persuading and training them is crucial due to their pioneering role in evidence implementation, especially change advancement. Consequently, local opinion leaders and “key individuals” were enrolled in the evidence-based practice team in this research to enhance their adaptability to innovation. Besides, the barriers from local opinion leaders were gradually dismantled through case teaching, negative examples, and personal interviews. Additionally, nurse managers exert a particularly influential role in implementing evidence-based practice.42 Therefore, it is vital to incorporate the head nurse as the project leader and a key facilitator with professional knowledge, evidence-based nursing experience, and management expertise. Because head nurses can mobilize necessary resources to facilitate evidence implementation, which is crucial for the success of this work.
Ultimately, the results of this research demonstrate the feasibility, appropriateness, clinical significance, and effectiveness of 6 audit criteria for OM prevention in children undergoing HSCT. At the system level, the OM nursing routine was revised, and toothbrush management schemes and a standardized workflow for oral cryotherapy were established, enhancing the standardization of nursing actions. Furthermore, the health education implementation scheme was refined and divided into sections for caregivers and children. For this purpose, age-appropriate health education materials and methods for pediatric patients were newly formulated under the scheme. At the nursing level, nurses became acquainted with implementation of evidence-based practice and recognized that medical practice should be grounded in the latest high-quality evidence despite a persist gap between the latest evidence and actual nursing practice.43 Integrating the evidence with practical knowledge and formulating audit criteria for clinical implementation has improved the compliance of clinical nurses with evidence-based nursing practice. At the patient level, the improvement of nurse compliance contributed to reducing the incidence of OM and lowering its severity.
Limitations
On the other hand, this research was subjected to several limitations. For example, it was implemented at a single center, the clinical evidence application lasted only two months, and the children enrolled were in a small size. Consequently, future research should be developed by involving multi-center evidence implementation, extending the duration, and making longer-term outcome observations to evaluate the perennial effectiveness of preventive measures for OM.
Conclusion
The objective of evidence translation is to integrate evidence for OM prevention in children undergoing HSCT into the clinical decision-making system, thereby guiding and sustaining effective nursing practices. This research identified and addressed the existing gaps between evidence and current clinical practice. By implementing evidence-based OM prevention measures, the study effectively standardized prevention protocols and nursing behaviors, solidified nursing habits, and enhanced clinical nurses’ adherence to best practices. Moreover, this study introduced novel contributions, including the development of child-specific cryotherapy methods and innovative health education formats aimed at improving children’s adherence to treatment. These tailored approaches not only increased compliance among pediatric patients but also significantly reduced the incidence and severity of OM, ultimately leading to higher-quality care for children. Moving forward, continuous quality improvement initiatives will be essential to further refine OM prevention strategies and sustain evidence-based nursing practices in pediatric HSCT settings.
Data Sharing Statement
The data and materials used in this study are available upon request. Researchers interested in accessing the dataset or related materials for academic and non-commercial purposes can contact the corresponding author for further information.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and was approved by Shenzhen Children’s Hospital, Shenzhen, Guangdong Province, People’s Republic of China.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Sanming Project of Medicine in Shenzhen SZSM202211033 Supported by Shenzhen Fund for Guangdong Provincial High-level Clinical Key Specialties (SZGSP012) Supported by Shenzhen Key Medical Discipline Construction Fund (SZXK034) Supported by Guangdong High-level Hospital Construction Fund Supported by Shenzhen High-level Hospital Construction Fund.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Stringer AM, Logan RM. The role of oral flora in the development of chemotherapy-induced oral mucositis. J Oral Pathol Med. 2015;44:81–87. doi:10.1111/jop.12152
2. Hong BY, Sobue T, Choquette L, et al. Chemotherapy-induced oral mucositis is associated with detrimental bacterial dysbiosis. Microbiome. 2019;7:66. doi:10.1186/s40168-019-0679-5
3. Feng Y, Pan LY, Shen LY, Chang PP, Zhang BH, Hong L. Changes in body composition in children with acute graft-versus-host disease within the first 100 days after hematopoietic stem cell transplantation. Eur J Clin Nutr. 2018;72:1167–1175. doi:10.1038/s41430-017-0057-y
4. Bardellini E, Schumacher F, Conti G, Porta F, Campus G, Majorana A. Risk factors for oral mucositis in children receiving hematopoietic cell transplantation for primary immunodeficiencies: a retrospective study. Pediatr Transplant. 2013;17:492–497. doi:10.1111/petr.12094
5. de Castro JF, Abreu EG, Correia AV, Da MVBC, Da CPD, de Paula RPF. Low-level laser in prevention and treatment of oral mucositis in pediatric patients with acute lymphoblastic leukemia. Photomed Laser Surg. 2013;31:613–618. doi:10.1089/pho.2012.3327
6. Vagliano L, Feraut C, Gobetto G, et al. Incidence and severity of oral mucositis in patients undergoing haematopoietic sct--results of a multicentre study. Bone Marrow Transplant. 2011;46:727–732. doi:10.1038/bmt.2010.184
7. Treister NS, London WB, Guo D, et al. A feasibility study evaluating extraoral photobiomodulation therapy for prevention of mucositis in pediatric hematopoietic cell transplantation. Photomed Laser Surg. 2016;34:178–184. doi:10.1089/pho.2015.4021
8. Miranda-Silva W, Da FF, Gomes AA, Mafra A, Rocha V, Fregnani ER. Oral mucositis in paediatric cancer patients undergoing allogeneic hematopoietic stem cell transplantation preventively treated with professional dental care and photobiomodulation: incidence and risk factors. Int J Paediatr Dent. 2022;32:251–263. doi:10.1111/ipd.12850
9. Curra M, Gabriel AF, Ferreira M, et al. Incidence and risk factors for oral mucositis in pediatric patients receiving chemotherapy. Support Care Cancer. 2021;29:6243–6251. doi:10.1007/s00520-021-06199-5
10. Oberoi S, Zamperlini-Netto G, Beyene J, Treister NS, Sung L. Effect of prophylactic low level laser therapy on oral mucositis: a systematic review and meta-analysis. PLoS One. 2014;9:e107418. doi:10.1371/journal.pone.0107418
11. Clarkson JE, Worthington HV, Furness S, Mccabe M, Khalid T, Meyer S. Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2010;2010:CD1973. doi:10.1002/14651858.CD001973.pub4
12. Worthington HV, Clarkson JE, Bryan G, et al. Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2011;2011:CD978. doi:10.1002/14651858.CD000978.pub5
13. Song JJ, Twumasi-Ankrah P, Salcido R. Systematic review and meta-analysis on the use of honey to protect from the effects of radiation-induced oral mucositis. Adv Skin Wound Care. 2012;25:23–28. doi:10.1097/01.ASW.0000410687.14363.a3
14. Patel P, Robinson PD, Baggott C, et al. Clinical practice guideline for the prevention of oral and oropharyngeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update. Eur J Cancer. 2021;154:92–101. doi:10.1016/j.ejca.2021.05.013
15. Sackett DL. Evidence-based medicine. Semin Perinatol. 1997;21:3–5. doi:10.1016/s0146-0005(97)80013-4
16. Gundogdu F, Sayar S. Oncology nursing practices in the management of chemotherapy-related oral mucositis in accordance with evidence-based guidelines: a descriptive and cross-sectional study. Support Care Cancer. 2022;30:9549–9557. doi:10.1007/s00520-022-07361-3
17. Cheng L, Broome ME, Feng S, Hu Y. Factors influencing the implementation of evidence in Chinese nursing practice. J Clin Nurs. 2017;26:5103–5112. doi:10.1111/jocn.14053
18. Williams B, Perillo S, Brown T. What are the factors of organisational culture in health care settings that act as barriers to the implementation of evidence-based practice? A scoping review. Nurse Educ Today. 2015;35:e34–e41. doi:10.1016/j.nedt.2014.11.012
19. Dicenso A, Bayley L, Haynes RB. Accessing pre-appraised evidence: fine-tuning the 5s model into a 6s model. Evid Based Nurs. 2009;12:99–101. doi:10.1136/ebn.12.4.99-b
20. Lizarondo L. Evidence summary. Hematopoietic stem cell transplantation: oral care. JBI EBP Database. 2021;2021:JBI–ES–4841–2.
21. Stephenson M. Evidence summary. Oral mucositis (pediatrics): prevention and management. JBI EBP Database. 2022;2022:JBI–ES–5118–1.
22. Brouwers MC, Kho ME, Browman GP, et al. Agree ii: advancing guideline development, reporting and evaluation in health care. Cmaj. 2010;182:E839–E842. doi:10.1503/cmaj.090449
23. Joanna Briggs Institute. The joanna briggs institute levels of evidence and grades of recommendation working party*. In: Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. Austrália: Joanna Briggs Institute; 2014.
24. Sonis ST, Elting LS, Keefe D, et al. Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epidemiology, and consequences for patients. Cancer. 2004;100:1995–2025. doi:10.1002/cncr.20162
25. Harvey G, Kitson A. Parihs revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11:33. doi:10.1186/s13012-016-0398-2
26. International Council of Nurses. Closing the gap: from evidence to action. Switzerland: ICN; 2012. Available from: https://www.nursingworld.org/~4aff6a/globalassets/practiceandpolicy/innovation--evidence/ind-kit-2012-for-nnas.pdf.
27. Pearson A, Jordan Z. Evidence-Based Clinical Practice in Nursing and Health Care: Assimilating Research, Experience and Expertise. Sydney: Wiley Blackwell; 2007:137–153.
28. Grossschadl F, Bauer S. The relationship between obesity and nursing care problems in intensive care patients in Austria. Nurs Crit Care. 2022;27:512–518. doi:10.1111/nicc.12554
29. Harvey GKA. Implementing Evidence-Based Practice in Healthcare: A Facilitation Guide. Abingdon, Oxon: Routledge; 2015:2–59.
30. Elad S, Cheng K, Lalla RV, et al. Mascc/isoo clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2020;126:4423–4431. doi:10.1002/cncr.33100
31. De Sanctis V, Bossi P, Sanguineti G, et al. Mucositis in head and neck cancer patients treated with radiotherapy and systemic therapies: literature review and consensus statements. Crit Rev Oncol Hematol. 2016;100:147–166. doi:10.1016/j.critrevonc.2016.01.010
32. Hong C, Gueiros LA, Fulton JS, et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27:3949–3967. doi:10.1007/s00520-019-04848-4
33. Cullen L, Baumler S, Farrington M, Dawson C, Folkmann P, Brenner L. Ce: oral care for head and neck cancer symptom management. Am J Nurs. 2018;118:24–34. doi:10.1097/01.NAJ.0000529694.30568.41
34. Hogan R. Implementation of an oral care protocol and its effects on oral mucositis. J Pediatr Oncol Nurs. 2009;26:125–135. doi:10.1177/1043454209334356
35. Huang TJ, Mu PF, Chen MB, Florczak K. Prevention and treatment of oral mucositis among cancer patients in the hematology-oncology setting: a best practice implementation project. Jbi Evid Implement. 2020;18:420–430. doi:10.1097/XEB.0000000000000238
36. van Leeuwen S, Potting C, Huysmans M, Blijlevens N. Salivary changes before and after hematopoietic stem cell transplantation: a systematic review. Biol Blood Marrow Transplant. 2019;25:1055–1061. doi:10.1016/j.bbmt.2019.01.026
37. Mccarthy GM, Awde JD, Ghandi H, Vincent M, Kocha WI. Risk factors associated with mucositis in cancer patients receiving 5-fluorouracil. Oral Oncol. 1998;34:484–490. doi:10.1016/s1368-8375(98)00068-2
38. Pimenta AT, Campos CC, Moreira DST, et al. Effect of salivary stimulation therapies on salivary flow and chemotherapy-induced mucositis: a preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:628–637. doi:10.1016/j.oooo.2011.10.012
39. Sung L, Robinson P, Treister N, et al. Guideline for the prevention of oral and oropharyngeal mucositis in children receiving treatment for cancer or undergoing haematopoietic stem cell transplantation. BMJ Support Palliat Care. 2017;7:7–16. doi:10.1136/bmjspcare-2014-000804
40. Jordan Z, Lockwood C, Munn Z, Aromataris E. Redeveloping the jbi model of evidence based healthcare. Int J Evid Based Healthc. 2018;16:227–241. doi:10.1097/XEB.0000000000000139
41. Aitken LM, Hackwood B, Crouch S, et al. Creating an environment to implement and sustain evidence based practice: a developmental process. Aust Crit Care. 2011;24:244–254. doi:10.1016/j.aucc.2011.01.004
42. Bianchi M, Bagnasco A, Bressan V, et al. A review of the role of nurse leadership in promoting and sustaining evidence-based practice. J Nurs Manag. 2018;26:918–932. doi:10.1111/jonm.12638
43. Jun J, Kovner CT, Stimpfel AW. Barriers and facilitators of nurses’ use of clinical practice guidelines: an integrative review. Int J Nurs Stud. 2016;60:54–68. doi:10.1016/j.ijnurstu.2016.03.006
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
