Back to Journals » Infection and Drug Resistance » Volume 17
Epidemiological Study on Case Definition of Methicillin-Resistant Staphylococcus aureus Enteritis
Authors Yagi Y , Doke A, Iwame S, Arakawa Y , Yamagishi Y
Received 15 January 2024
Accepted for publication 17 May 2024
Published 4 June 2024 Volume 2024:17 Pages 2237—2247
DOI https://doi.org/10.2147/IDR.S459708
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yusuke Yagi,1,2 Akito Doke,1,3 Saya Iwame,1,3 Yu Arakawa,1,4 Yuka Yamagishi1,4
1Department of Infection Prevention and Control, Kochi Medical School Hospital, Nankoku, Kochi, Japan; 2Department of Pharmacy, Kochi Medical School Hospital, Nankoku, Kochi, Japan; 3Department of Clinical Laboratory, Kochi Medical School Hospital, Nankoku, Kochi, Japan; 4Department of Clinical Infectious Diseases, Kochi Medical School, Kochi University, Nankoku, Kochi, Japan
Correspondence: Yuka Yamagishi, Department of Clinical Infectious Diseases, Kochi Medical School, Kochi University, Nankoku, Kochi, 783-8505, Japan, Tel +81 88 866 5811, Fax +81 88 880 2611, Email [email protected]
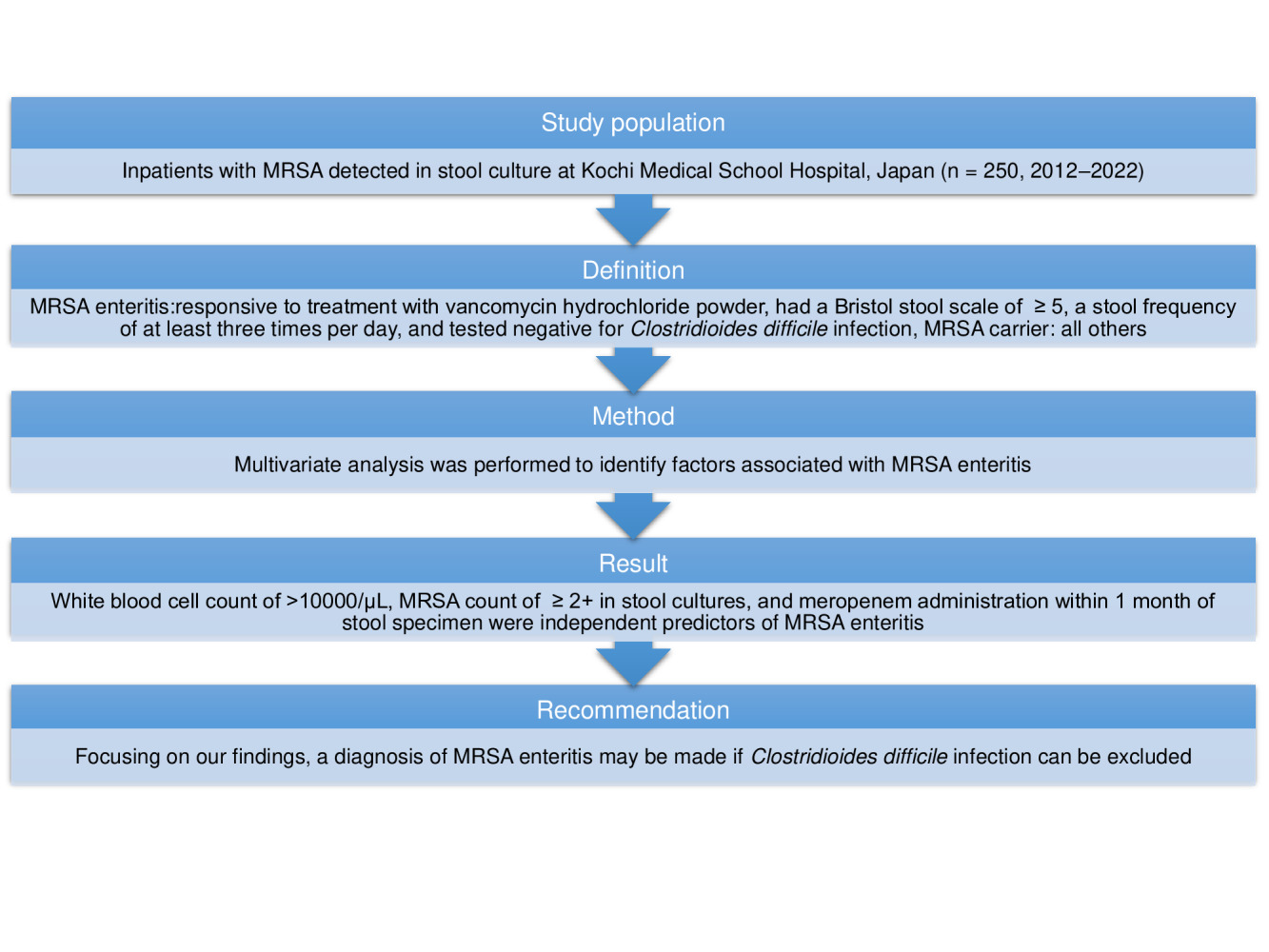
Background: Methicillin-resistant Staphylococcus aureus (MRSA) enteritis is a condition in which MRSA grows abnormally in the intestine after administration of antimicrobial agents, resulting in enteritis. Patients with MRSA detected in stool culture tests are often diagnosed with MSRA enteritis. However, uncertainty remains in the diagnostic criteria; therefore, we conducted epidemiological studies to define these cases.
Patients and Methods: Patients who tested positive for MRSA by stool culture using selective media 48 h after admission to Kochi Medical School Hospital between April 1, 2012, and December 31, 2022, and did not meet the exclusion criteria were included. We defined MRSA enteritis (Group A) as cases that were responsive to treatment with vancomycin hydrochloride powder, had a Bristol Stool Scale of ≥ 5, and a stool frequency of at least three times per day; all others were MRSA carriers (Group B). Multivariate analysis was performed to risk factors associated with MRSA enteritis.
Results: Groups A and B included 18 (25.4%) and 53 (74.6%) patients, respectively. Multivariate logistic regression analysis showed that a white blood cell count of > 10000/μL (odds ratio [OR], 5.50; 95% confidence interval [CI], 1.12– 26.9), MRSA count of ≥ 2+ in stool cultures (OR, 8.91; 95% CI, 1.79– 44.3), and meropenem administration within 1 month of stool specimen submission (OR, 7.47; 95% CI, 1.66– 33.6) were risk factors of MRSA enteritis.
Conclusion: The case definitions reviewed for MRSA enteritis may be useful as diagnostic criteria.
Keywords: MRSA enteritis, diagnostic criteria, white blood cell, MRSA counts in stool cultures, meropenem
Graphical Abstract:
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is the most frequently isolated nosocomial antibiotic-resistant bacterium and a problematic organism in healthcare-associated infections.1 MRSA enteritis is a condition in which MRSA grows abnormally in the intestine after administration of antimicrobial agents, resulting in enteritis. Patients with MRSA detected in stool culture tests are often diagnosed with MRSA enteritis.2,3 In Japan, MRSA enteritis is characterized by profuse watery diarrhea and has been reported to occur in older individuals, postoperatively in patients who underwent gastrectomy, and immunocompromised patients, and as a bacterial shift phenomenon after the administration of third-generation cephalosporin antibacterial agents.4 Furthermore, MRSA enteritis was most frequently observed in the late 1980s and the early 1990s,5,6 and since then, severe cases and deaths due to MRSA enteritis have become rare, and the number of cases has markedly decreased.7 In addition, while the efficacy of screening for MRSA using chromogenic media has been reported, its diagnostic utility remains uncertain.8 This is due to the lack of a firm definition of MRSA enteritis, which is caused by a lack of definition of diarrheal symptoms and frequency, inadequate studies on the number of MRSA detected, lack of routine examination of virulence factors and lack of pathological studies.9 In contrast, Clostridioides difficile infection (CDI) is often observed in healthcare facilities,10 and appropriate diagnostic criteria have been established.11 Uncertainty remains in the diagnostic criteria of MRSA enteritis; therefore, we considered that a case definition for the diagnostic criteria of MRSA enteritis was required. We retrospectively examined the clinical characteristics and associated factors of cases where MRSA was detected in stool culture tests.
Materials and Methods
Study Design and Patients
This retrospective cohort study was conducted at Kochi Medical School Hospital between April 1, 2012, and December 31, 2022.
Patients who tested positive for MRSA after submitting a diarrhea stool specimen were included. If the same patient submitted multiple stool specimens between admission and discharge, only the first submission was considered.
The exclusion criteria were as follows: age < 18 years, patients who submitted a stool specimen within 48 h of admission, patients who received laxatives or intestinal decongestant cleansing agents within 48 h of the date of stool specimen submission, patients who received tube feeding for > 31 days within 1 month of the date of stool specimen submission, and patients with underlying inflammatory bowel disease. The Bristol Stool Scale (BSS) is a diagnostic medical tool used in clinical practice to classify human fecal morphology into seven categories.12 In this study, after referring to previous reports,12,13 we defined MRSA enteritis (Group A) as cases that were responsive to treatment with vancomycin hydrochloride powder and had a BSS of at least 5 and a stool frequency of at least 3 times per day, whereas MRSA carriers (Group B) were defined as cases that did not receive vancomycin hydrochloride powder and did not have a BSS of at least 5 or stool frequency of at least 3 times per day.
Data Collection
Clinical data were reviewed from electronic medical records to obtain complete medical records when MRSA was detected in patients’ stool samples.
Information obtained from the electronic medical records included age, sex, route of admission, number of days from admission to stool examination, and relevant symptoms (eg, abdominal symptoms and fever) at the time of stool specimen submission. Furthermore, the data included autonomous defecation, underlying or comorbid conditions, biochemical or hematological tests, endoscopic findings, bacteria detected concurrent with MRSA in stool specimens, detection of MRSA in all specimens within 14 days of stool specimen submission. Data on antimicrobials, antacid preparations, intestinal regulating drugs, enteral nutrition, gastrointestinal surgery, cancer chemotherapy and radiation therapy, vancomycin hydrochloride administration, death within 28 days of stool specimen submission, and death during hospitalization were also collected.
Microbiological Examinations
Within 2 h of receiving the specimens at the hospital, we inoculated approximately 1 g of stool specimen on agar media. The type of media and incubation conditions are as follows: MRSA I-A agar (Nikken Seibutsu Co., Ltd., Japan),14 BTB lactose agar (Becton Dickinson), CHROMagarTM candida/potato dextrose fractionated medium (Kanto Chemical Co., Inc., Japan), CHROMagarTM STEC/SSV fractionated medium (Kanto Chemical Co., Inc., Japan), Pearlcore® TCBS agar medium “Eiken” (Eiken Chemical Co., Ltd., Japan), Pearlcore® SS agar medium “Eiken” (Eiken Chemical Co., Ltd., Japan) at 37°C for 48 h in an aerobic environment, and Campylobacter 10% sheep blood agar (Becton Dickinson) at 35°C for 48 h in a microaerophilic culture. MRSA I-A agar can concurrently screen clinical specimens for Staphylococcus aureus and MRSA using egg yolk reaction for determination.14 Based on colonies developed on MRSA I-A agar, the number of bacteria was expressed in semiquantitative quantities as 1+, 2+, 3+, and 4+. The number of bacteria by semiquantitative quantification was determined to correspond to the following bacterial abundance: 1+ = 103 to 104 colony forming units (CFU)/mL, 2+ = 104 to 105 CFU/mL, 3+ = 105 to 106 CFU/mL, and 4+ = > 106 CFU/mL. Bacterial species were identified based on biochemical properties from April 2012 to July 2022 and using matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI Biotyper ver. 9.0.0.0; Bruker Daltonics, Billerica, MA, USA) after August 2022. Antimicrobial susceptibility testing was performed using the microdilution method, and the results were interpreted according to the most recent Clinical and Laboratory Standards Institute Guidelines 2021.15 Colonies that developed on MRSA I-A agar were subjected to antimicrobial susceptibility tests using the Microscan Pos Series with Combo Panel (Beckman Coulter, Inc., USA). The inoculum was standardized to a density of 0.5 McFarland standard by prompt method. Susceptibility to 15 antimicrobial agents (benzylpenicillin, ampicillin, oxacillin, sulbactam/ampicillin, clavulanic acid/amoxicillin, gentamicin, erythromycin, clarithromycin, minocycline, levofloxacin, vancomycin, daptomycin, sulfamethoxazole-trimethoprim, rifampicin, and linezolid) was assessed. The MRSA strain was used for quality control. The toxin was confirmed to diagnose CDI using a rapid immunoenzyme test for glutamate dehydrogenase and toxin (TECHLAB C. Diff Quik Chek COMPLETE kit, TECHLAB, Inc., USA). For glutamate dehydrogenase (+) and toxin (-) detection, the samples were applied to Accurate™ CCMA medium EX (Shimadzu Diagnostics, Inc., Tokyo, Japan). The strains were then coated with Accurate™ CCMA medium EX (Shimadzu Diagnostics, Inc., Tokyo, Japan) and incubated at 35°C for 48 h under anaerobic conditions. The developed strains were tested using the same kits.
All samples were analyzed using quantitative cytomegalovirus real-time polymerase chain reaction on a Cobas 6800 system (Roche Diagnostics, USA).
Variable Definitions
Continuous variables were divided into the following categories: age (</≥ 65 years),16 Charlson Comorbidity Index (0, 1–2, 3–4, ≥ 5),17 albumin (</≥ 3.0 g/dL),18 C-reactive protein (CRP) (</≥ 6.1 mg/dL), creatinine (male: </≥ 1.07, female: </≥ 0.79),18 estimated glomerular filtration rate (≤/> 60 mL/min/1.73 m2),19 white blood cell (WBC) (≤/>10000 /µL),20 and MRSA counts in stool culture (1+, ≥ 2+).9,21 The cut-off point for CRP was set to the median value, while age, Charlson Comorbidity Index, albumin level, creatinine level, WBC count, estimated glomerular filtration rate, and MRSA counts in stool culture were set based on the respective guidelines and literature.15–21
Statistical Analysis
Categorical variables are reported as percentages and continuous variables are reported as medians and interquartile ranges.22 All statistical analyses were performed using EZR version 1.29 (Saitama Medical Center, Jichi Medical University, Saitama, Japan).23 Fisher’s exact test (two-tailed) was used to compare categorical variables, and the Mann–Whitney U-test was used to compare continuous variables. Logistic regression analysis was used to identify independent factors associated with diarrhea in patients with MRSA enteritis. Variables with P < 0.05 in univariate analysis were entered into a multivariate model. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for each variable in the multivariate model. Statistical significance was set at P < 0.05.
Ethics Statement
This study was approved by the Ethical Review Board of Kochi University School of Medicine (registration number: ERB-109102). All procedures adhered to the tenets of the Declaration of Helsinki. Informed consent was exempted from obtaining because no invasion or intervention on the patients and only medical and other information was used to conduct the study. Information on the conduct of the study was disclosed and patients were given the opportunity to refuse.
Results
Seventy-one patients who tested positive for MRSA using stool culture and did not meet the exclusion criteria were included in the study (Figure 1). The overall patient characteristics are summarized in Table 1. They were older (71.8 years) and predominantly male (64.8%). Stomachache (80.3%) and fever (temperature ≥ 38.0°C) (64.8%) were the most common accompanying symptoms at the time of stool specimen submission. The patient backgrounds of Group A and Group B are shown in Table 1. The results of microbiology examinations, including the MRSA counts in stool culture and details of the bacteria detected along with MRSA, are presented in Table 2. Group A included 18 patients (25.4%), and Group B included 53 patients (74.6%). Group A patient had significantly higher CRP levels (P = 0.01), WBC counts (P = 0.01), and MRSA counts of ≥2+ in stool cultures (44.4%, P = 0.02) than Group B patients. Moreover, a higher number of Group A patients had MRSA detected in sputum within 14 days of stool specimen submission (50.0%, P < 0.01) and meropenem administration within 1 month of stool specimen submission than Group B patients (55.6%, P < 0.01) (Table 2). The antimicrobial susceptibility profiles of MRSA isolates are shown in Table 3.
 |
Table 1 Comparison of Patient Characteristics Between Group A and Group B |
 |
Table 2 Microbiological Examinations Between Groups A and B |
 |
Table 3 Antimicrobial Susceptibility of MRSA Strains Between Groups A and B |
Multivariate logistic regression analysis showed that WBC counts of >10000 /µL (OR, 5.50; 95% CI, 1.12–26.9; P = 0.04), MRSA counts of ≥ 2+ in stool cultures (OR, 8.91; 95% CI, 1.79–44.3; P < 0.01), and meropenem administration within 1 month of stool specimen submission (OR, 7.47; 95% CI, 1.66–33.6; P < 0.01) remained risk factors for diarrhea development (Table 4). In contrast, CRP > 6.1 mg/dL and retrospective detection of MRSA in sputum within 14 days from the date of stool culture submission were not associated with diarrhea (Table 4).
 |
Table 4 Multivariate Analysis of Patients’ Background Risk Factors |
Discussion
MRSA enteritis was reported as a postoperative complication with a high mortality rate in Japan in the 1990s.5,6 Diarrhea and fever were the main symptoms, and most cases occurred after gastrectomy or colorectal resection.2–4 In Japan, there have been no reports of MRSA enteritis since 2002.18 The exclusion of CDI is important for the diagnosis of MRSA enteritis because of its history, which suggests that culture-positive C. difficile for MRSA may have been misidentified as antibiotic-associated enterocolitis due to MRSA.24 C. difficile-positive patients were excluded from this study.
In this study, 27.8% of patients in Group A underwent gastrectomy or colorectal resection. The disease was thought to be caused by early postoperative immune compromise of host-side antibodies due to exotoxins, such as enterotoxin and toxic shock syndrome toxin 1.
In previous reports, the mean age ranged from 51 to 72 years, and the patients we reviewed were older, with similar results.2,3,25,26 The background of patients diagnosed with MRSA enteritis included sex differences and reported history of gastrointestinal surgery.2,3 The results were similar for groups that fit the case definition of MRSA enteritis in our study, which was more common in males (71.4%) than in females. The results were not statistically significant in terms of surgical history. Men and women have different immunocompetencies,27 men have a lower humoral immune response than women due to lower antibody production by B cells,28 and androgens and sex steroid hormones are thought to be involved.29
Diarrheal stools due to MRSA enteritis have been reported to be watery; however, there have been no reports on the frequency of stools. Simultaneous evaluation of diarrheal appearance and frequency of stools, as defined in this study, would be a useful diagnostic tool for MRSA enteritis. In case reports of MRSA enteritis, endoscopic findings indicate that the small intestine is the primary site of the lesion.30 Therefore, MRSA enteritis is considered a non-inflammatory small intestinal type of enteritis, and it has been inferred that fecal leukocytes are not as significant as those in colonic enteritis. In the present study, we were unable to examine the fecal leukocytes. However, in previous reports, MRSA enteritis was diagnosed when the blood leukocyte count exceeded 10000 /μL or decreased below 3100 /μL.26,27 In our study, MRSA enteritis was associated with a blood leukocyte count exceeding 10000 /μL. This leukocytosis may be related to granulocyte colony-stimulating factor production from stromal cells and monocytes due to MRSA-derived enterotoxin.31 Granulocyte colony-stimulating factor was found in 3 (16.7%) of the 18 MRSA enteritis cases.
Fecal specimens from patients with diarrhea that developed after 3 days of hospitalization had a low yield when tested for standard bacterial pathogens.32,33 Based on this finding, several groups have suggested that unless overriding circumstances prevail, fecal specimens from patients hospitalized for > 3 days should not be subjected to routine stool culture.34,35 However, in our study, only patients who submitted stool cultures > 3 days after admission were selected and tested using MRSA selective media for rapid detection of infected patients.
The detection of MRSA and the number of MRSA bacteria in the stool culture are important for diagnosing MRSA enteritis, given the possibility that a stool culture would be necessary. The criterion for bacterial abundance was ≥ 104 to 105 CFU/mL, that is, high bacterial abundance. Ogawa et al diagnosed MRSA enteritis when the amount of MRSA bacteria in the stool culture was 104 CFU/mL.9 Our study finding was similar, concluding that an MRSA bacterial level of 104 to 105 CFU/mL or higher was required.
In all but one case, other bacteria detected concurrently with MRSA in stool specimens were commensal intestinal bacteria. A small number of C. difficile were detected in Groups A and B. Based on the results of rapid immunoenzyme tests, these organisms were considered carriers. No pathogenic enterohemorrhagic Escherichia coli, Salmonella species, or cytomegalovirus was detected. The antimicrobial susceptibility results of MRSA revealed that all strains were completely resistant to oxacillin. Conversely, several strains were found to be sensitive to erythromycin, clarithromycin, clindamycin, and levofloxacin only in Group B. The susceptibility pattern suggested community-acquired MRSA.36
Antimicrobial exposure is a risk factor for diarrhea, especially with broad-spectrum antimicrobials.37 In our study, previously reported third-generation cephalosporins were not identified as associated factors.4 When tested retrospectively for 1 month from the date of diarrhea onset as an exposure history, meropenem was found to cause significant diarrhea. Thus, past exposure history can be a risk factor, and we emphasize the importance of reviewing dosing history. A broad-spectrum antimicrobial agent, such as meropenem, which has antimicrobial activity against an entire range of aerobic and anaerobic bacteria in the intestinal tract, can cause bacterial turnover in the intestinal tract, resulting in MRSA enteritis.38
This study has several limitations. First, this was a retrospective study with a relatively small number of patients. Therefore, it was impossible to corroborate the histological findings. Endoscopic findings were obtained in one case and were not abnormal. Pseudomembrane formation in the small intestine may be a hallmark of MRSA enteritis, and endoscopy and case series are required for its diagnosis.39,40 Second, we were unable to examine MRSA-derived toxins that may cause enterocolitis; enterotoxin A and toxic shock syndrome toxin 1 involvement are thought to be responsible for the severity of MRSA enterocolitis.7,41 Molecular genetic studies are required to examine these diagnostic criteria. Despite these limitations, this is the first study to evaluate the factors involved in defining MRSA enteritis aimed at confirming its existence in hospitals.
Conclusion
MRSA enteritis may be diagnosed when diarrhea occurs, WBC count is >10000 /µL, and MRSA count in stool cultures is ≥ 2+. The history of meropenem use in the past 1 month should also be considered. These diagnostic criteria would allow clinicians to identify patients with diarrhea-onset disease likely to develop MRSA enteritis. A multicenter study will be conducted in the future to increase the number of cases studied and to evaluate the diagnostic ability of the risk factors identified in our study. Moreover, whenever possible, we will examine the causes of pathogenicity and pathologic underpinnings in MRSA enteritis.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Author Contributions
All authors made significant contributions in the conception, study design, implementation, data acquisition, analysis, interpretation, or all of these areas; drafted or wrote the article or performed critical peer review; reviewed and agreed to any significant changes made in the final version approved for publication and in the proofreading stage; agreed to the journal to which they submitted the paper; and accepted responsibility for all aspects of the research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Turner NA, Sharma-Kuinkel BK, Maskarinec SA, et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol. 2019;17:203–218. doi:10.1038/s41579-018-0147-4
2. Kodama T, Santo T, Yokoyama T, et al. Postoperative enteritis caused by methicillin-resistant Staphylococcus aureus. Surg Today. 1997;27:816–825. doi:10.1007/BF02385272
3. Takeuchi K, Tsuzuki Y, Ando T, et al. Clinical studies of enteritis caused by methicillin-resistant Staphylococcus aureus. Eur J Surg. 2001;167:293–296. doi:10.1080/110241501300091507
4. Hori K, Yura J, Shinagawa N, Sakurai S, Mashita K, Mizuno A. Postoperative enterocolitis and current status of MRSA enterocolitis–the result of a questionnaire survey in Japan. Kansenshogaku Zasshi. 1989;63:701–707. doi:10.11150/kansenshogakuzasshi1970.63.701
5. Iwai S, Sato T, Kunimatsu M, et al. Hospital acquired infection in surgical field and its countermeasure present situation of anaerobes, P. aeruginosa and MRSA infection. Nihon Geka Gakkai Zasshi. 1992;93:906–909.
6. Iwai S, Akutsu M. Severe infection in gastroenterological field; MRSA (methicillin resistant Staphylococcus aureus) enterocolitis. Nihon Rinsho. 1994;52:456–461.
7. Okii K, Hiyama E, Takesue Y, Kodaira M, Sueda T, Yokoyama T. Molecular epidemiology of enteritis-causing methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2006;62:37–43. doi:10.1016/j.jhin.2005.05.013
8. Dodémont M, Verhulst C, Nonhoff C, et al. Prospective two-center comparison of three chromogenic agars for methicillin-resistant Staphylococcus aureus screening in hospitalized patients. J Clin Microbiol. 2015;53:3014–3016. doi:10.1128/JCM.01006-15
9. Ogawa Y, Saraya T, Koide T, et al. Methicillin-resistant Staphylococcus aureus enterocolitis sequentially complicated with septic arthritis: a case report and review of the literature. BMC Res Notes. 2014;7:21. doi:10.1186/1756-0500-7-21
10. Curry SR, Muto CA, Schlackman JL, et al. Use of multilocus variable number of tandem repeats analysis genotyping to determine the role of asymptomatic carriers in Clostridium difficile transmission. Clin Infect Dis. 2013;57:1094–1102. doi:10.1093/cid/cit475
11. Kunishima H, Ohge H, Suzuki H, et al. Japanese Clinical Practice Guidelines for Management of Clostridioides (Clostridium) difficile infection. J Infect Chemother. 2022;28:1045–1083. doi:10.1016/j.jiac.2021.12.011
12. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920–924. doi:10.3109/00365529709011203
13. World Health Organization. Diarrhoea. Available from: http://www.who.int/topics/diarrhoea/en/. (
14. Nikken Seibutsu Co. Ltd. Japan. MRSA I-A agar; 2021. Available from: http://www.nikken-bio.co.jp/product/pamphlet/100.pdf.
15. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. M100‑S31. Wayne, PA: CLSI; 2021.
16. Arai H. Definition of older people: time to reconsider the definition? Nihon Ronen Igakkai Zasshi. 2019;56:1–5.
17. de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol. 2003;56:221–229. doi:10.1016/S0895-4356(02)00585-1
18. National Institutes of Health National Cancer Institute (2009). common terminology criteria for adverse events (CTCAE) Version 4.0 [PDF file]. Available at: https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/Archive/CTCAE_4.0_2009-05-29_QuickReference_5x7.pdf.
19. Imai E, Horio M, Watanabe T, et al. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol. 2009;13:621–630. doi:10.1007/s10157-009-0199-x
20. George EL, Panos A. Does a high WBC count signal infection? Nursing. 2005;35:20–21. doi:10.1097/00152193-200501000-00014
21. Ohge H, Yokoyama T, Shimizu W, et al. MRSA enteritis. Is it truth? J Jpn Soc Surg Infect. 2012;9:171–175.
22. Matsuo S, Aihara M, Takahashi H. Clinical and pathological study of 34 patients with isolation of methicillin-resistant Staphylococcus aureus in stool culture. Kansenshogaku Zasshi.1991;65:1394–1402. doi:10.11150/kansenshogakuzasshi1970.65.1394
23. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–458. doi:10.1038/bmt.2012.244
24. Bartlett JG. Antibiotic-associated diarrhea. N Engl J Med. 2002;346:334–339. doi:10.1056/NEJMcp011603
25. Sekikawa T. The study of cases with infection by methicillin-resistant Staphylococcus aureus. Rinsho Byori. 1990;38:1211–1218.
26. Haq AI, Cook LJ. MRSA enteritis causing a high stoma output in the early postoperative phase after bowel surgery. Ann R Coll Surg Engl. 2007;89:303–308. doi:10.1308/003588407X179143
27. Klein SL. The effects of hormones on sex differences in infection: from genes to behavior. Neurosci Biobehav Rev. 2000;24:627–638. doi:10.1016/S0149-7634(00)00027-0
28. Schuurs AH, Verheul HA. Effects of gender and sex steroids on the immune response. J Steroid Biochem. 1990;35:157–172. doi:10.1016/0022-4731(90)90270-3
29. Olsen NJ, Kovacs WJ. Gonadal steroids and immunity. Endocr Rev. 1996;17:369–384. doi:10.1210/edrv-17-4-369
30. Fujita K, Honda Y, Kurihara T, Ohba H, Okimoto N. A case of pseudomembranous enterocolitis caused by methicillin-resistant Staphylococcus aureus. Kansenshogaku Zasshi. 2004;78:905–909. doi:10.11150/kansenshogakuzasshi1970.78.905
31. Hartung T, Döcke WD, Gantner F, et al. Effect of granulocyte colony-stimulating factor treatment on ex vivo blood cytokine response in human volunteers. Blood. 1995;85:2482–2489. doi:10.1182/blood.V85.9.2482.bloodjournal8592482
32. Siegel DL, Edelstein PH, Nachamkin I. Inappropriate testing for diarrheal diseases in the hospital. JAMA. 1990;263:979–982. doi:10.1001/jama.1990.03440070067034
33. Hines J, Nachamkin I. Effective use of the clinical microbiology laboratory for diagnosing diarrheal diseases. Clin Infect Dis. 1996;23:1292–1301. doi:10.1093/clinids/23.6.1292
34. Morris AJ, Wilson ML, Reller LB. Application of rejection criteria for stool ovum and parasite examinations. J Clin Microbiol. 1992;30:3213–3216. doi:10.1128/jcm.30.12.3213-3216.1992
35. Fan K, Morris AJ, Reller LB. Application of rejection criteria for stool cultures for bacterial enteric pathogens. J Clin Microbiol. 1993;31:2233–2235. doi:10.1128/jcm.31.8.2233-2235.1993
36. Piao C, Karasawa T, Totsuka K, et al. Prospective surveillance of community-onset and healthcare-associated methicillin-resistant Staphylococcus aureus isolated from a university-affiliated hospital in Japan. Microbiol Immunol. 2005;49:959–970. doi:10.1111/j.1348-0421.2005.tb03691.x
37. Koizumi Y, Kimura T, Hatanaka S, Kadotani M, Takahashi Y. Risk factors for the induction of antibiotic-associated diarrhea. Kankyokansenshi. 2008;23:175–180.
38. Yang JJ, Wang JT, Cheng A, Chuang YC, Sheng WH. Impact of broad-spectrum antimicrobial treatment on the ecology of intestinal flora. J Microbiol Immunol Infect. 2018;51:681–687. doi:10.1016/j.jmii.2016.12.009
39. Wakefield RD, Sommers SC. Fatal membranous staphylococcal enteritis in surgical patients. Ann Surg. 1953;138(2):249–252. doi:10.1097/00000658-195308000-00011
40. Altemeier WA, Hummel RP, Hill EO. Staphylococcal enterocolitis following antibiotic therapy. Ann Surg. 1963;157:847–858. doi:10.1097/00000658-196306000-00003
41. Uchiyama T, Yan XJ, Imanishi K, Yagi J. Bacterial superantigens--mechanism of T cell activation by the superantigens and their role in the pathogenesis of infectious diseases. Microbiol Immunol 1994. 38:245–256 doi:doi: 10.1111/j.1348-0421.1994.tb01772.x..
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

