Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 19
Higher Vitamin E Intake Reduces Risk of All-Cause Mortality and Chronic Lower Respiratory Disease Mortality in Chronic Obstructive Pulmonary Disease: NHANES (2008–2018)
Authors Tian M, Li W, He X, He Q, Huang Q, Deng Z
Received 12 March 2024
Accepted for publication 12 August 2024
Published 21 August 2024 Volume 2024:19 Pages 1865—1878
DOI https://doi.org/10.2147/COPD.S468213
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Maoliang Tian,1,* Wenqiang Li,1,* Xiaoyu He,2 Qian He,3 Qian Huang,4 Zhiping Deng1
1Zigong First People’s Hospital, Zigong City, Sichuan Province, 643000, People’s Republic of China; 2North Sichuan Medical College, Nanchong, Sichuan Province, 637000, People’s Republic of China; 3West China Second Hospital of Sichuan University, Chengdu, Sichuan Province, 610044, People’s Republic of China; 4Dazhou Dachuan District People’s Hospital (Dazhou Third People’s Hospital), Dazhou, Sichuan Province, 635000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qian Huang, Dazhou Dachuan District People’s Hospital (Dazhou Third People’s Hospital), Dazhou, Sichuan Province, 635000, People’s Republic of China, Email [email protected] Zhiping Deng, Zigong First People’s Hospital, Zigong City, Sichuan Province, 643000, People’s Republic of China, Email [email protected]
Background: In human health, vitamins play a vital role in various metabolic and regulatory processes and in the proper functioning of cells. Currently, the effect of Vitamin E (VE) intake on multiple causes of death in Chronic obstructive pulmonary disease (COPD) patients is unclear. Therefore, this paper aims to investigate the relationship between VE and multiple causes of death in COPD patients, to guide the rationalization of dietary structure and reduce the risk of COPD death.
Methods: This study screened patients with COPD aged ≥ 40 years from the National Health and Nutrition Examination Survey (NHANES) database 2008– 2018. Weighted COX regression was used to analyze the association between VE intake and multiple causes of death in COPD. The restricted cubic spline(RCS) is drawn to show their relationship. Finally, we conducted a subgroup analysis for further verification.
Results: A total of 1261 participants were included in this study. After adjustment for multiple covariates, VE intake was associated with all-cause death in COPD patients, and chronic lower respiratory disease (CLRD) deaths were linearly associated with cardiovascular disease (CVD) deaths there was no such correlation. Subgroup analyses showed no interaction between subgroups, further validating the robustness of the relationship.
Conclusion: In COPD patients, VE intake was negatively associated with all-cause mortality and CLRD death. Higher VE intake reduces the risk of all-cause mortality and CLRD death in COPD patients.
Keywords: vitamin E, COPD, CVD, CLRD, COX regression analyses
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous lung condition characterised by chronic respiratory symptoms, usually manifesting as persistent, progressively worsening airflow obstruction.1 It often occurs in the 40–50 years of age.2 In 2019, according to the global initiative for chronic obstructive lung disease (GOLD), the global prevalence of COPD was approximately 10%, totaling nearly 400 million people.3 Over time, the economic burden of COPD will increase due to the persistence of risk factors and the aging population.1 Currently, cardiovascular disease (CVD) and chronic lower respiratory disease (CLRD) dominate multiple causes of death globally.4–7 People with COPD die not only because of an acute exacerbation, but about two-thirds die from extrapulmonary causes, such as CVD and cancer.8 CVD is the most common cause of death from extrapulmonary causes, accounting for 16–39% of all deaths.9–11
Diet is recognized as a modifiable risk factor for the development and progression of chronic diseases.12 As an important part of the diet, vitamins are divided into fat-soluble vitamins and water-soluble vitamins, which are essential for normal cell function, growth and development.13,14 So deficiencies in these micronutrients can lead to a variety of clinical abnormalities, and optimizing levels in the body can lead to positive health outcomes.15,16 So far, studies have confirmed that vitamins A, C, D, E, B2, B6, and B12 are closely related to the regulation of immunity.17,18 Supplementation of appropriate vitamins can help the body improve immune function and reduce the impact of pathogen infection, which is a universal anti-infection program with feasibility and effectiveness in lung infections.18,19 At the same time, for other causes of oxidative stress in the lungs, healthy dietary patterns and specific nutrient intake can reduce its response, thereby reducing the damage to the body.20,21
In COPD, there have been previous studies of vitamin E (VE) in relation to disease.22–24 It has also been shown that VE is associated with lung function and cardiovascular disease.25–27 However, there are no studies examining the association between VE and all-cause, CVD, and CLRD deaths in COPD patients. For the first time, we examined the association between VE intake and all-cause, CVD, and CLRD deaths in COPD patients by combining the contents of the National Health and Nutrition Examination Survey (NHANES) database, which included COPD patients aged 40 years and older.
Research Design and Methods
Population Studied
The NHANES is a long-term, stratified, multistage sample study in which data are obtained through interviews and physical examinations. Therefore, the NHANES database has the advantages of large sample size, rich information sources, follow-up information and reliable data, and is open to all researchers. The database is conducted every 2 years, and about 5000 people across the country are surveyed each year. And all participants signed an informed consent form provided by the NHANES Ethics Review Committee.
We selected COPD (n = 2244) from 2008–2018 (5 cycles) in NHANES (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx). Exclusion criteria were (1) no follow-up information (n = 9); (2) <40 years of age (n = 89); (3) pregnant or with a tumor at the time of the cross-sectional survey (n = 832); and (4) missing values (n = 414). Ultimately, we included a total of 1261 COPD for analysis (Figure 1).
 |
Figure 1 Participant selection process. |
Definition of COPD
The definition of COPD was mainly based on pulmonary function tests, COPD questionnaire reports (MCQ160G, MCQ160P) and medication use.
- FEV1/FVC <0.7 after inhaled bronchodilators.
- Have you been diagnosed with emphysema in the past? (MCQ160G, MCQ160P)
- Use of medications for COPD (leukotriene modulators, inhaled corticosteroids, selective phosphodiesterase-4 inhibitors, mast cell stabilizers)? In addition, history of smoking or chronic bronchitis, age over 40 years.
VE Intake
NHANES staff obtained the type and amount of food and beverages (including all types of water) consumed by participants in the 24 hours prior to the inquiry through an interview format. They were further processed into the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS) to assess the intake of energy, nutrients, and other food components in these foods and beverages. We obtained information on the daily dietary VE content from NHANES, which was transformed it into log2 for analysis due to its large value.
Covariate Indicators
NHANES staff obtained information through standardized questionnaires on age group (40–64 or ≥65), sex (male or female), marriage (married/living with partner, never married or widowed/divorced/separated), race (white or other), insurance status (yes or no), drinking status (yes or no), smoking status (former, never or now), body mass index (BMI) (<30 or ≥30), education level (high school diploma, lower than high school or more than high school), poverty income ratio (PIR) (≥3 or <3), hypertension (yes or no), and diabetes mellitus (pre-diabetes, yes or no). PIR ranges from 0 (no family income) to 5 (family income at least five times the annual federal poverty level). Insurance status specifically refers to whether or not family insurance is purchased. Smoking is categorized as non-smoking, former smoking, and current smoking. They were defined as having smoked fewer than 100 cigarettes in their lifetime, more than 100 cigarettes but not currently smoking, and having smoked more than 100 cigarettes and still smoking, respectively.28 BMI is weight/height2 (kg/m2), and ≥30 kg/m2 is considered obese.
Study Outcome
The outcome is death or end of follow-up. As of December 31, 2019, as determined by the National Death Index Record, whichever arrives first.CVD death codes are E10-E14, I00-I09, I11, I13, I60-I69, N00-N07, N17-N19, N25-N27.CLRD death codes are J09-J18, J40-J47.
Statistical Analysis
The NHANES database used a complex sampling design and constructed sample weights to obtain a nationally representative sample. Appropriate weights (1/10 × wtmec2yr) were selected based on the study factors and results of this study, and the results of the following statistical analyses were based on the weighting of the data. All statistical analyses were performed using R software version 4.2.1, and P < 0.05 (two-sided) was considered statistically significant. The optimal cut-off value for VE that was most significantly associated with survival outcomes was determined using the maximum selected rank statistics method (MSRSM) and divided into high and low VE groups according to this value. Continuous variables were expressed as weighted means and standard deviations, and categorical variables were expressed as weighted percentages. We compared differences between groups using the chi-square test. We then assessed the hazard ratio (HR) of daily dietary VE content to all-cause, CVD, and CLRD mortality in COPD using weighted multivariate COX regression models and calculated 95% confidence intervals (CIs).
We analyzed three model outcomes for each death outcome. Model 1 was fitted for age, gender, race, marriage, and education. Model 2 adjusted for smoking, alcohol consumption, PIR and insurance factors on the basis of Model 1. Model 3 also adjusted for hypertension and diabetes factors on top of Model 2. We then plotted restricted cubic spline (RCS) to explore the dose-response associations between VE and the risk of all-cause, CVD, and CLRD mortality in COPD. Kaplan-Meier method was used to analyze the survival differences of COPD causes of death between the high and low VE groups. Finally, we further stratified analyses by sex, age, race, marriage, smoking status, drinking status, and education level. Potential modification effects were examined by multiplicative interaction tests.
Results
Baseline Characteristic
Among 1261 COPD patients aged 40 years and older, the median follow-up time was 8.25 years. As can be observed from Table 1, COPD often occurs in people who are 40–64 years old, male, married or in cohabitation, highly educated, former or current smokers, drinkers, and often uncomplicated with obesity and diabetes. The optimal log2-VE cutoff value (3.36) was determined according to MSRSM (Figure 2), and participants were divided into high VE intake group (log2-VE≥3.36) and low VE intake group (log2-VE<3.36). COPD was more likely to occur in those with low VE intake, and VE intake was lower in those with all-cause, CVD, and CLRD deaths compared with those who survived, implying that VE intake may be negatively associated with all-cause, CVD, and CLRD deaths in COPD patients. Regardless of the levels of vitamins A, B6, B12, and C, there was no significant difference in the distribution of all-cause, CVD, and CLRD mortality among COPD patients.
 |
Table 1 Baseline Characteristics of Participants in NHANES 2008–2018 |
 |
Figure 2 The MSRSM method divides vitamin E into the high and low vitamin E groups. |
Association of VE with All-Cause Mortality in COPD
Among 1261 COPD, 791 survived (median follow-up time of about 9.58 years) and 470 died (median follow-up time of about 5.54 years). Table 2 demonstrates the Results of our analysis of the association between log2-VE and all-cause mortality in COPD patients using weighted multifactorial COX regression, which ultimately revealed a negative association between log2-VE and all-cause mortality in COPD after stepwise adjustments in several models (all P < 0.05). In the complete model, HR in the high-VE group was 0.64 (0.44, 0.92) and P = 0.02 compared to the low-VE group. log2-VE remained negatively associated with all-cause death in COPD (HR: 0.86, 95% CI: 0.77–0.97, P = 0.01), suggesting that the risk of all-cause death in COPD patients was reduced by 14% for every unit increase in log2-VE. The RCS plot also visualized a negative linear association between log2-VE and all-cause mortality in COPD (Figure 3A). Kaplan-Meier analysis showed a difference in survival in terms of all-cause death between the high and low VE groups (P < 0.001), with higher survival in the high VE group (Figure 4A).
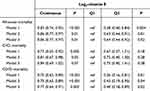 |
Table 2 Association of Vitamin E with Risk of COPD All-Cause, CVD, and CLRD Mortality |
 |
Figure 3 Association between vitamin E intake and risk of COPD all-cause (A) and CLRD (B) mortality in the 2008-2018 NHANES survey. |
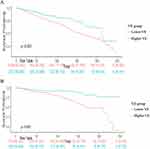 |
Figure 4 Difference in survival between high and low vitamin E groups of COPD patients. (A) all-cause mortality. (B) CLRD mortality. |
Additionally, we conducted subgroup analyses for groups without and with adjustments for other vitamins (Vitamins A, B6, B12, C), categorized by age, sex, marital status, race, smoking status, alcohol consumption, BMI, and education level. We found that in the group without adjustments for other vitamins, the relationship between Vitamin E intake and all-cause mortality in COPD patients showed no significant interactions among the subgroups except for BMI (all P > 0.05). In the group with adjustments for other vitamins, there were no significant interactions among the subgroups (all P > 0.05) (Table 3). The subgroup analysis results were generally consistent between the two groups, suggesting that the intake of other vitamins does not confound the relationship between Vitamin E intake and all-cause mortality risk in COPD patients. Moreover, after adjusting for other vitamins, statistical significance was observed in the subgroups of those who were married or had a partner, had never smoked, and had an education level above high school, where the intake of other vitamins could influence the effect of Vitamin E on the prognosis of all-cause mortality in COPD patients (Table 3).
 |
Table 3 Stratified Analysis of the Association Between Vitamin E and Risk of All-Cause Mortality in COPD |
Association of VE with CVD Mortality in COPD
153 out of 1261 participants died of CVD with a median follow-up time of approximately 5.17 years. The results in Table 2 show that in the final model, there was no significant association between log2-VE and CVD deaths in COPD patients, either in continuous values or in subgroups (HR 0.84 (0.69, 1.02), 0.75 (0.40, 1.41), respectively, both P > 0.05).
Association of VE with CLRD Mortality in COPD
120 of 1261 COPD patients died of CLRD with a median follow-up of approximately 6.67 years. Multifactorial COX regression analysis showed a negative correlation between both log2-VE and death from CLRD in COPD patients (all P < 0.05) (Table 2). In the complete model, HR in the high-VE group was 0.40 (0.18, 0.89) and P = 0.02 compared to the low-VE group (Table 2). And log2-VE remained negatively associated with CLRD death in COPD (HR: 0.77, 95% CI: 0.64–0.91, P = 0.003), suggesting that for every unit increase in log2-VE, the risk of CLRD death in COPD patients was reduced by 23% (Table 2). The RCS plot also visualized a negative linear association between log2-VE and CLRD death in COPD (Figure 3B). The Kaplan-Meier survival curve showed that CLRD mortality was lower in the high-VE group than in the low-VE group (P < 0.001) (Figure 4B).
Additionally, we conducted subgroup analyses for groups without and with adjustments for other vitamins (Vitamin A, B6, B12, C), categorized by age, sex, race, smoking status, BMI, and education level. The results indicated that, regardless of adjustments for other vitamins, the relationship between Vitamin E intake and CLRD mortality risk in COPD patients remained consistent, with no significant interactions among the subgroups (all P > 0.05) (Table 4). The subgroup analysis results were generally consistent between the two groups, suggesting that the intake of other vitamins does not confound the relationship between Vitamin E intake and CLRD mortality risk in COPD patients. Moreover, after adjusting for other vitamins, statistical significance was observed in the subgroups aged ≥65 years or with a BMI ≥30 kg/m², where the intake of other vitamins could influence the effect of Vitamin E on CLRD mortality prognosis in COPD patients (Table 4).
 |
Table 4 Stratified Analysis of the Association Between Vitamin E and Risk of CLRD Mortality in COPD |
Discussion
For this study, we utilized the NHANES database, which is rich in content, scientific, and reliable. Previous studies have found that VE intake is positively associated with lung function25 and negatively associated with the risk of COPD.23 Our study confirmed that dietary VE intake was also inversely associated with all-cause and CLRD deaths in COPD, with a significant dose-response relationship through a generalized additive model. There was no significant correlation with CVD death in COPD patients.
COPD is a leading cause of morbidity, mortality and healthcare consumption worldwide,29 which is caused by exposure to inhaled toxic particles, especially tobacco smoke and pollutants.30 In recent years, increasing attention has been paid to a wide range of factors that increase the risk of COPD development and progression throughout the life course, including early lung development and infection.1 Dietary factors might modulate the effects of adverse environmental exposures or genetic predisposition on the lungs, but may also have direct (protective or harmful) effects on biological processes involved in lung function, disease development and outcome.31–33
Vitamins are a group of organic compounds that are essential to the physiological functioning of the body. Vitamin content has a positive significance in the development of the lungs and already plays a role in the development of the foetal lungs during pregnancy.34,35 At the same time, vitamins, as the main dietary nutrients, are the regulatory factors of immune response, and their influence on human immunity is crucial.36 Pulmonary respiratory infection in childhood has an important influence on the trajectory of pulmonary function changes in adults and can increase the prevalence of COPD.37 Dietary interventions early in life may help lung function remain stable throughout life. What’s more, in a randomised trial, the role of vitamin C in preventing acute respiratory infections (ARI) was stronger in men and middle-income countries compared with adult women and high-income countries, respectively.38 During COVID-19, a controlled study confirmed that supplementation with 1 g/d vitamin C reduced symptoms and shortened disease duration, thereby improving recovery rates.39
At present, a number of studies have shown that nutrient intake affects the occurrence of many diseases and deaths.40–44 The beneficial effects of nutrition on lung health have also been well explored. Certain micronutrients and phytochemicals have been shown to have anti-inflammatory and antioxidant properties that directly target the pathogenesis of decreased lung function.45,46 Vitamins A, B6, B12, C, D and E are common anti-inflammatory and antioxidant nutrients. A meta-analysis of 44 randomized controlled trials showed that vitamin C reduced all-cause mortality in adults.44 Another systematic review of 19 randomized controlled trials showed that vitamin A supplementation in children reduced morbidity and mortality.43 High serum levels of vitamin D reduce all-cause and CVD mortality in osteoarthritis.40 In addition, serum antioxidant vitamin levels may also affect lung disease prognosis. A large study in the United States showed that low serum levels of vitamins A, C, D, and E increase the incidence of respiratory disease in addition to mortality in adults.47
VE has antioxidant and anti-inflammatory properties. These characteristics may affect the occurrence, progression and prognosis of COPD.48,49 The occurrence and deterioration of COPD are related to oxidative stress, inflammatory cytokine release, protease activity and autoantibody expression.50 Oxidative stress occurs when reactive oxygen species (ROS) overwhelm the body’s antioxidant defense system, damaging DNA, proteins, and lipids, leading to cellular damage and even death.51 The lungs are susceptible to oxidative stress because of their hyperoxic environment, abundant blood flow, and susceptibility to exposure to pathogens and toxins.51 ROS predispose to lung injury. Messier et al established a mouse model and found that water-soluble VE derivatives could prevent lung injury by clearing ROS against oxidative stress, genotoxicity and inflammation.52 Zhao et al showed that VE can negatively regulate EGFR/MAPK signaling, reduce ROS, anti-inflammatory and anti-apoptosis, and inhibit Cox2-mediated phosphorylated STAT3 translocation to alleviate COPD.53
Currently, there are no studies investigating the association between VE and the risk of all-cause, CVD, and CLRD mortality in COPD patients. To fill this gap, we conducted a large-sample analysis using the NHANES database. The results showed a significant negative correlation between VE intake and the risk of all-cause and CLRD mortality in the COPD population, demonstrating a dose-response relationship. Higher VE intake was associated with a reduced risk of all-cause and CLRD mortality in COPD patients. However, no significant association was found with CVD mortality risk. VE is known to have antioxidant properties and is hypothesized to protect the cardiovascular system by inhibiting oxidative stress, which is inconsistent with our study’s findings. However, numerous high-quality studies have also shown that there is no significant association between VE and the risk or mortality of CVD.54–56 The specific mechanisms underlying this lack of association remain unclear but may be related to two factors: On one hand, VE might reduce the size of high-density lipoprotein (HDL) through unknown gene regulation, thereby increasing the risk of CVD.57,58 On the other hand, Vitamin E may induce the production of CYP3A4 or MDR1, thereby reducing the efficacy of certain cardiovascular drugs.56 Therefore, it is not necessarily beneficial for cardiovascular mortality. From our study, it is hypothesized that eating as many VE-rich foods as possible is beneficial in reducing the risk of COPD all-cause and CLRD deaths, especially in the middle-aged population.
Previous studies have shown that certain vitamins may interact with each other. Low-dose VE combined with other vitamins or minerals can reduce individual or all-cause mortality.59 Tocopherols and tocotrienols are the most bioavailable forms of VE in the body, acting as free radical scavengers on the surface of biological membranes, removing fatty acid peroxyl radicals, and generating tocopherol radicals, which can be reduced by vitamin C or ubiquinol to regenerate VE.60,61 In our study, subgroup analysis comparing adjusted and unadjusted groups for other vitamins (A, B6, B12, C) showed that the relationship between vitamin E and all-cause or CLRD mortality in COPD patients remained consistent across subgroups, indicating no confounding effect from other vitamins. However, for all-cause mortality, after adjusting for other vitamins, statistical significance was observed in the subgroups of married or partnered individuals, never smokers, and those with a high school education or higher. In these three subgroups, the intake of other vitamins affected prognosis. In CLRD mortality, after adjusting for other vitamins, statistical significance was observed in the subgroups aged ≥65 years or with a BMI ≥30 kg/m², where the intake of other vitamins affected prognosis. More fundamental research on the interactions between different vitamins is urgently needed. Understanding these interactions is crucial for developing comprehensive nutritional guidelines and therapeutic strategies, particularly for patients with chronic conditions such as COPD.
The strengths of this study are that it includes a large, nationally representative sample and that subgroup analyses were conducted. Inevitably, of course, it also has certain limitations. First, although NHANES has improved questionnaire reliability through regular training of investigators and other measures, recall bias and self-report bias still exist. In order to reduce this bias and improve the reliability of the conclusion, combined with the age characteristics of people with a high incidence of COPD, we selected people aged 40 years and above as researchers. Second, although we adjusted for the possible presence of confounders such as basic information and underlying disease, we could not avoid the presence of residual confounders. Finally, and more importantly, the vitamins were derived from the results of the 1-day questionnaire, and it was not possible to assess any changes over time.
Abbreviations
COPD, Chronic obstructive pulmonary disease; GLOD, global initiative for chronic obstructive lung disease; CVD, cardiovascular disease; CLRD, chronic lower respiratory disease; VE, vitamin E; NHANES, National Health and Nutrition Examination Survey; FNDDS, Food and Nutrient Database for Dietary Studies; BMI, body mass index; PIR, Poverty-to-income ratios; MSRSM, maximum selected rank statistics method; HR, hazard ratio; CIs, confidence intervals; RCS, restricted cubic spline; ARI, acute respiratory infections; ROS, reactive oxygen species; HDL, high-density lipoprotein.
Data Sharing Statement
The dataset for this study can be found on the NHANES website NHANES - National Health and Nutrition Examination Survey Homepage (cdc.gov).
Ethics Approval and Consent to Participate
Article 32 of the “Ethical Review Methods for Life Sciences and Medical Research Involving Humans“ stipulates: ”Research that meets the following criteria does not require ethical approval: (a) uses legally obtained public data, or data generated through observation that does not interfere with public behavior; (b) uses anonymous information data for research”. This study uses data from a legally public database—the NHANES database (The research protocol of NHANES has been approved by the Research Ethics Review Board (ERB) of the National Center for Health Statistics (NCHS), and participants provided written informed consent at the time of registration). Additionally, this study uses anonymous information data for research, and therefore does not require ethical approval and consent. The Medical Ethics Committee of the Zigong First People’s Hospital exempted this study (Ethics number: 2024-029).
Acknowledgments
The authors would like to thank all the staff of the NHANES for their contributions to the Human Health and Nutrition Status Research Program. Thanks to Zhang Jing (Second Department of Infectious Disease, Shanghai Fifth People’s Hospital, Fudan University) for his work on the NHANES database. His outstanding work, nhanesR package and webpage, makes it easier for us to explore NHANES database.
Author Contributions
Maoliang Tian and Wenqiang Li designed the study. Qian He extracted data from NHANES set. Wenqiang Li analyzed the data. Xiaoyu He drew figures and tables. Maoliang Tian and Qian Huang wrote the manuscript. Qian Huang and Zhiping Deng reviewed the manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Key Science and Technology Project of Zigong City, Sichuan Province (grant no. ZGYKY22KF001).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Global Initiative for Chronic Obstructive Lung Disease.Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease(2023 Report). Available from: https://goldcopd.org/2023-gold-report-2/#.
2. Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet. 2015;385(9971):899–909. doi:10.1016/S0140-6736(14)60446-3
3. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–458. doi:10.1016/S2213-2600(21)00511-7
4. Pająk A, Jankowski P, Zdrojewski T. The burden of cardiovascular disease risk factors: a current problem. Kardiol Pol. 2022;80(1):5–15. doi:10.33963/KP.a2022.0018
5. Lee YC, Chang KY, Sethi S. Association of chronic lower respiratory disease with. COUNTY Health Disparities in New York State. JAMA Netw Open. 2021;4(11):e2134268.
6. Oelsner EC, Loehr LR, Henderson AG, et al. Classifying chronic lower respiratory disease events in epidemiologic cohort studies. Ann Am Thorac Soc. 2016;13(7):1057–1066. doi:10.1513/AnnalsATS.201601-063OC
7. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
8. Shu CC, Lee JH, Tsai MK, Su TC, Wen CP. The ability of physical activity in reducing mortality risks and cardiovascular loading and in extending life expectancy in patients with COPD. Sci Rep. 2021;11(1):21674. doi:10.1038/s41598-021-00728-2
9. Gulea C, Zakeri R, Kallis C, Quint JK. Impact of COPD and asthma on in-hospital mortality and management of patients with heart failure in England and Wales: an observational analysis. BMJ Open. 2022;12(6):e059122. doi:10.1136/bmjopen-2021-059122
10. Wise RA, Anzueto A, Cotton D, et al. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369(16):1491–1501. doi:10.1056/NEJMoa1303342
11. Berry CE, Wise RA. Mortality in COPD: causes, risk factors, and prevention. COPD. 2010;7(5):375–382. doi:10.3109/15412555.2010.510160
12. Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ. 2018;361:
13. Godoy-Parejo C, Deng C, Zhang Y, Liu W, Chen G. Roles of vitamins in stem cells. Cell Mol Life Sci. 2020;77(9):1771–1791. doi:10.1007/s00018-019-03352-6
14. Osman DE, Phon BWS, Kamarudin MNA, Ponnampalam SN, Radhakrishnan AK, Bhuvanendran S. Biomarkers regulated by lipid-soluble vitamins in glioblastoma. Nutrients. 2022;14(14):2873. doi:10.3390/nu14142873
15. Fandiño J, Toba L, González-Matías LC, Diz-Chaves Y, Mallo F. Perinatal undernutrition, metabolic hormones, and lung development. Nutrients. 2019;11(12):2870. doi:10.3390/nu11122870
16. Cook-Mills JM, Averill SH, Lajiness JD. Asthma, allergy and vitamin E: current and future perspectives. Free Radic Biol Med. 2022;179:388–402. doi:10.1016/j.freeradbiomed.2021.10.037
17. Bhaskaram P. Micronutrient malnutrition, infection, and immunity: an overview. Nutr Rev. 2002;60(5):S40–45. doi:10.1301/00296640260130722
18. Yuan X, Duan Y, Xiao Y, et al. Vitamin E enhances cancer immunotherapy by reinvigorating dendritic cells via targeting checkpoint SHP1. Cancer Discov. 2022;12(7):1742–1759. doi:10.1158/2159-8290.CD-21-0900
19. Jolliffe DA, Camargo CA, Sluyter JD, et al. Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials. Lancet Diabetes Endocrinol. 2021;9(5):276–292. doi:10.1016/S2213-8587(21)00051-6
20. de Batlle J, Barreiro E, Romieu I, et al. Dietary modulation of oxidative stress in chronic obstructive pulmonary disease patients. Free Radic Res. 2010;44(11):1296–1303. doi:10.3109/10715762.2010.500667
21. van Iersel LEJ, Beijers R, Gosker HR, Schols A. Nutrition as a modifiable factor in the onset and progression of pulmonary function impairment in COPD: a systematic review. Nutr Rev. 2022;80(6):1434–1444. doi:10.1093/nutrit/nuab077
22. Wu TC, Huang YC, Hsu SY, Wang YC, Yeh SL. Vitamin E and vitamin C supplementation in patients with chronic obstructive pulmonary disease. Internat J Vitamin Nutrit Res Internationale Zeitschrift Fur Vit. 2007;77(4):272–279. doi:10.1024/0300-9831.77.4.272
23. Liu Z, Su Y, Chen Q, et al. Association of Dietary intake of vitamin E with chronic obstructive pulmonary disease events in US adults: a cross-sectional study of NHANES 2013-2018. Front Nutr. 2023;10:1124648. doi:10.3389/fnut.2023.1124648
24. Daga MK, Chhabra R, Sharma B, Mishra TK. Effects of exogenous vitamin E supplementation on the levels of oxidants and antioxidants in chronic obstructive pulmonary disease. J Biosci. 2003;28(1):7–11. doi:10.1007/BF02970125
25. Hanson C, Lyden E, Furtado J, et al. Serum tocopherol levels and vitamin E intake are associated with lung function in the normative aging study. Clin Nutr. 2016;35(1):169–174. doi:10.1016/j.clnu.2015.01.020
26. Sozen E, Demirel T, Ozer NK. Vitamin E: regulatory role in the cardiovascular system. IUBMB Life. 2019;71(4):507–515. doi:10.1002/iub.2020
27. Violi F, Nocella C, Loffredo L, Carnevale R, Pignatelli P. Interventional study with vitamin E in cardiovascular disease and meta-analysis. Free Radic Biol Med. 2022;178:26–41. doi:10.1016/j.freeradbiomed.2021.11.027
28. Navaneethan SD, Mandayam S, Arrigain S, Rahman M, Winkelmayer WC, Schold JD. Obstructive and restrictive lung function measures and CKD: national Health and Nutrition Examination Survey (NHANES) 2007-2012. Am J Kidney Dis. 2016;68(3):414–421. doi:10.1053/j.ajkd.2016.03.415
29. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. 2022;399(10342):2227–2242. doi:10.1016/S0140-6736(22)00470-6
30. Golpe R, Sanjuán López P, Cano Jiménez E, Castro Añón O, Pérez de Llano LA. Distribution of clinical phenotypes in patients with chronic obstructive pulmonary disease caused by biomass and tobacco smoke. Arch Bronconeumol. 2014;50(8):318–324. doi:10.1016/j.arbres.2013.12.013
31. Whyand T, Hurst JR, Beckles M, Caplin ME. Pollution and respiratory disease: can diet or supplements help? A review. Respir Res. 2018;19(1):79. doi:10.1186/s12931-018-0785-0
32. Smit HA. Chronic obstructive pulmonary disease, asthma and protective effects of food intake: from hypothesis to evidence? Respir Res. 2001;2(5):261–264. doi:10.1186/rr65
33. Zhai T, Li S, Hu W, Li D, Leng S. Potential micronutrients and phytochemicals against the pathogenesis of chronic obstructive pulmonary disease and lung cancer. Nutrients. 2018;10(7):813. doi:10.3390/nu10070813
34. McEvoy CT, Shorey-Kendrick LE, Milner K, et al. Effect of vitamin C supplementation for pregnant smokers on offspring airway function and wheeze at age 5 years: follow-up of a randomized clinical trial. JAMA Pediatr. 2023;177(1):16–24. doi:10.1001/jamapediatrics.2022.4401
35. Maden M. Retinoids in lung development and regeneration. Curr Top Dev Biol. 2004;61:153–189.
36. Chen HY, Hsu M, Lio CJ. Micro but mighty-Micronutrients in the epigenetic regulation of adaptive immune responses. Immunol Rev. 2022;305(1):152–164. doi:10.1111/imr.13045
37. de Marco R, Accordini S, Marcon A, et al. Risk factors for chronic obstructive pulmonary disease in a European cohort of young adults. Am J Respir Crit Care Med. 2011;183(7):891–897. doi:10.1164/rccm.201007-1125OC
38. Abioye AI, Bromage S, Fawzi W. Effect of micronutrient supplements on influenza and other respiratory tract infections among adults: a systematic review and meta-analysis. BMJ Glob Health. 2021;6(1):e003176. doi:10.1136/bmjgh-2020-003176
39. Hemilä H, Carr A, Chalker E. Vitamin C may increase the recovery rate of outpatient cases of SARS-CoV-2 Infection by 70%: reanalysis of the COVID A to Z randomized clinical trial. Front Immunol. 2021;12:674681. doi:10.3389/fimmu.2021.674681
40. Wang J, Fan J, Yang Y, et al. Vitamin D status and risk of all-cause and cause-specific mortality in osteoarthritis patients: results from NHANES III and NHANES 2001-2018. Nutrients. 2022;14(21):1.
41. Chen F, Du M, Blumberg JB, et al. Association among dietary supplement use, nutrient intake, and mortality among U.S. adults: a cohort study. Ann Intern Med. 2019;170(9):604–613. doi:10.7326/M18-2478
42. Somoza-Moncada MM, Turrubiates-Hernández FJ, Muñoz-Valle JF, et al. Vitamin D in depression: a potential bioactive agent to reduce suicide and suicide attempt risk. Nutrients. 2023;15(7):1765. doi:10.3390/nu15071765
43. Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2017;3(3):Cd008524. doi:10.1002/14651858.CD008524.pub3
44. Xu C, Yi T, Tan S, et al. Association of oral or intravenous vitamin C supplementation with mortality: a systematic review and meta-analysis. Nutrients. 2023;15(8):1848. doi:10.3390/nu15081848
45. Schünemann HJ, Freudenheim JL, Grant BJ. Epidemiologic evidence linking antioxidant vitamins to pulmonary function and airway obstruction. Epidemiol Rev. 2001;23(2):248–267. doi:10.1093/oxfordjournals.epirev.a000805
46. Durham AL, Adcock IM. The relationship between COPD and lung cancer. Lung Cancer. 2015;90(2):121–127. doi:10.1016/j.lungcan.2015.08.017
47. Salo PM, Mendy A, Wilkerson J, et al. Serum antioxidant vitamins and respiratory morbidity and mortality: a pooled analysis. Respir Res. 2022;23(1):150. doi:10.1186/s12931-022-02059-w
48. Zheng L, Yu X, Xia Z, Guo Y, Dai Y. The associations between serum vitamins and carotenoids with chronic obstructive pulmonary disease: results from the NHANES. Int J Chron Obstruct Pulmon Dis. 2023;18:2985–2997. doi:10.2147/COPD.S432995
49. Walda IC, Tabak C, Smit HA, et al. Diet and 20-year chronic obstructive pulmonary disease mortality in middle-aged men from three European countries. Eur J Clin Nutr. 2002;56(7):638–643. doi:10.1038/sj.ejcn.1601370
50. Brusselle GG, Joos GF, Bracke KR. New insights into the immunology of chronic obstructive pulmonary disease. Lancet. 2011;378(9795):1015–1026. doi:10.1016/S0140-6736(11)60988-4
51. McGuinness AJ, Sapey E. Oxidative Stress in COPD: sources, Markers, and Potential Mechanisms. J Clin Med. 2017;6(2):21. doi:10.3390/jcm6020021
52. Messier EM, Bahmed K, Tuder RM, Chu HW, Bowler RP, Kosmider B. Trolox contributes to Nrf2-mediated protection of human and murine primary alveolar type II cells from injury by cigarette smoke. Cell Death Dis. 2013;4(4):e573–e573. doi:10.1038/cddis.2013.96
53. Zhao H, Gong J, Li L, et al. Vitamin E relieves chronic obstructive pulmonary disease by inhibiting COX2-mediated p-STAT3 nuclear translocation through the EGFR/MAPK signaling pathway. Lab Invest. 2022;102(3):272–280. doi:10.1038/s41374-021-00652-z
54. Buijsse B, Feskens EJ, Kwape L, Kok FJ, Kromhout D. Both alpha- and beta-carotene, but not tocopherols and vitamin C, are inversely related to 15-year cardiovascular mortality in Dutch elderly men. J Nutr. 2008;138(2):344–350. doi:10.1093/jn/138.2.344
55. O’Connor EA, Evans CV, Ivlev I, et al. Vitamin and mineral supplements for the primary prevention of cardiovascular disease and cancer: updated evidence report and systematic review for the US preventive services task force. JAMA. 2022;327(23):2334–2347. doi:10.1001/jama.2021.15650
56. Clarke MW, Burnett JR, Croft KD. Vitamin E in human health and disease. Crit Rev Clin Laborat Sci. 2008;45(5):417–450. doi:10.1080/10408360802118625
57. Rainwater DL, Mahaney MC, VandeBerg JL, Wang XL. Vitamin E dietary supplementation significantly affects multiple risk factors for cardiovascular disease in baboons. The American Journal of Clinical Nutrition. 2007;86(3):597–603. doi:10.1093/ajcn/86.3.597
58. Buring JE, O’Connor GT, Goldhaber SZ, et al. Decreased HDL2 and HDL3 cholesterol, Apo A-I and Apo A-II, and increased risk of myocardial infarction. Circulation. 1992;85(1):22–29. doi:10.1161/01.CIR.85.1.22
59. Jiang S, Pan Z, Li H, Li F, Song Y, Qiu Y. Meta-analysis: low-dose intake of vitamin E combined with other vitamins or minerals may decrease all-cause mortality. J Nutrit Sci Vitaminol. 2014;60(3):194–205. doi:10.3177/jnsv.60.194
60. Neubauer O, Yfanti C. Antioxidants in Athlete’s Basic Nutrition: considerations towards a Guideline for the Intake of Vitamin C and Vitamin E. In: Lamprecht M, editor. Antioxidants in Sport Nutrition. Boca Raton (FL): CRC Press/Taylor & Francis; 2015.
61. Higgins MR, Izadi A, Kaviani M. Antioxidants and exercise performance: with a focus on Vitamin E and C supplementation. Int J Environ Res Public Health. 2020;17(22):8452. doi:10.3390/ijerph17228452
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
