Back to Journals » International Journal of Nanomedicine » Volume 19
Nanoenzymes: A Radiant Hope for the Early Diagnosis and Effective Treatment of Breast and Ovarian Cancers
Authors Shahid S, Khan A, Shahid W, Rehan M, Asif R, Nisar H, Kanwal Q , Choi JR
Received 22 January 2024
Accepted for publication 16 April 2024
Published 13 June 2024 Volume 2024:19 Pages 5813—5835
DOI https://doi.org/10.2147/IJN.S460712
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Eng San Thian
Samiah Shahid,1,2 Ayesha Khan,1 Wajeehah Shahid,3 Mehvesh Rehan,2 Roha Asif,1 Haseeb Nisar,4 Qudsia Kanwal,5 Jeong Ryeol Choi6
1Research Centre for Health Sciences (RCHS), The University of Lahore, Lahore, Pakistan; 2Institute of Molecular Biology and Biotechnology (IMBB), The University of Lahore, Lahore, Pakistan; 3Department of Physics, The University of Lahore, Lahore, Pakistan; 4School of Life Sciences, University of Management and Technology, Lahore, Pakistan; 5Department of Chemistry, The University of Lahore, Lahore, Pakistan; 6School of Electronic Engineering, Kyonggi University, Suwon, Kyeonggi-do, 16227, Republic of Korea
Correspondence: Samiah Shahid, Research Centre for Health Sciences (RCHS), Associate Professor, Institute of Molecular Biology and Biotechnology (IMBB), The University of Lahore, Lahore, 54590, Pakistan, Email [email protected] Jeong Ryeol Choi, School of Electronic Engineering, Kyonggi University, Suwon, Kyeonggi-do, 16227, Republic of Korea, Email [email protected]
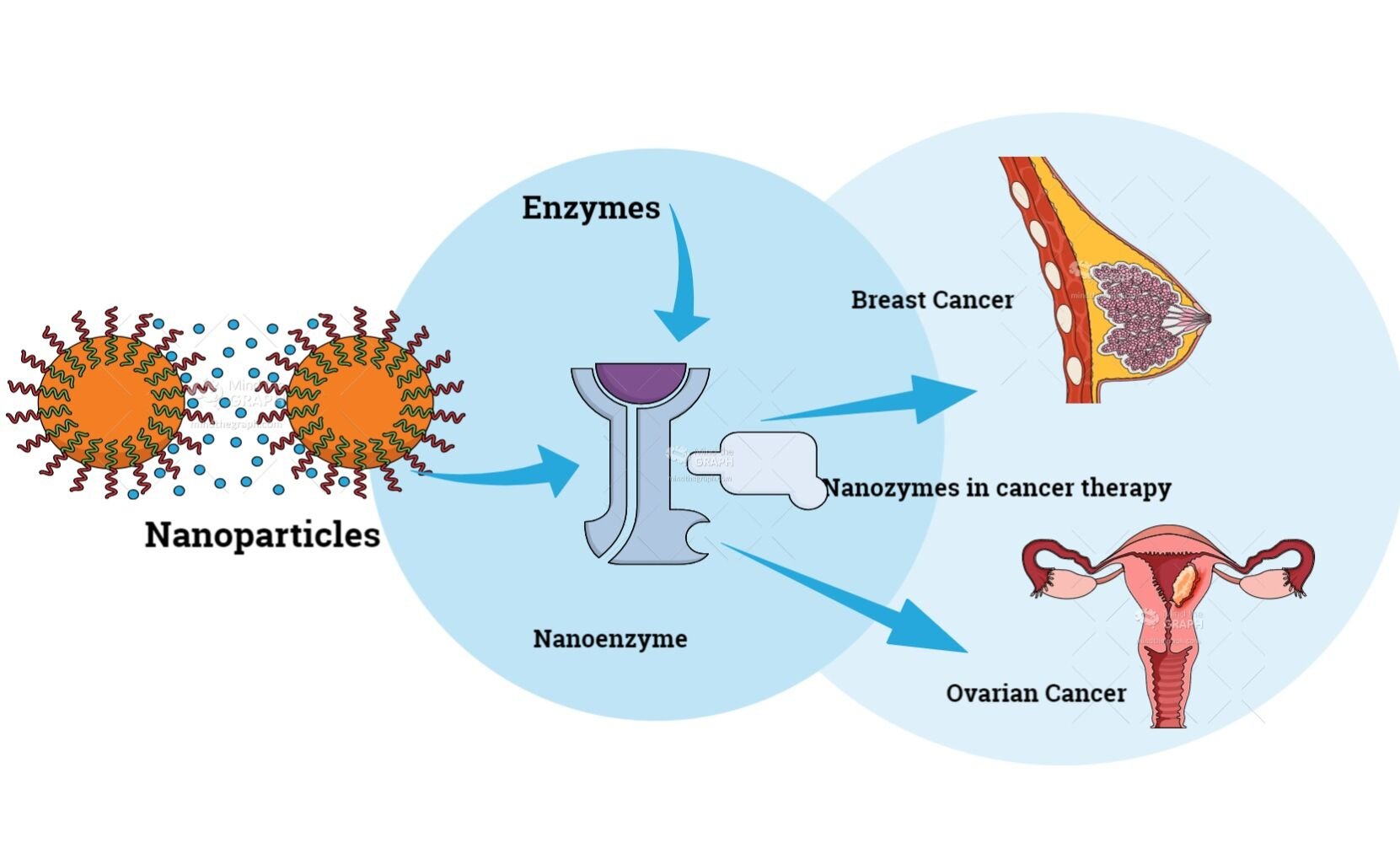
Abstract: Breast and ovarian cancers, despite having chemotherapy and surgical treatment, still have the lowest survival rate. Experimental stages using nanoenzymes/nanozymes for ovarian cancer diagnosis and treatment are being carried out, and correspondingly the current treatment approaches to treat breast cancer have a lot of adverse side effects, which is the reason why researchers and scientists are looking for new strategies with less side effects. Nanoenzymes have intrinsic enzyme-like activities and can reduce the shortcomings of naturally occurring enzymes due to the ease of storage, high stability, less expensive, and enhanced efficiency. In this review, we have discussed various ways in which nanoenzymes are being used to diagnose and treat breast and ovarian cancer. For breast cancer, nanoenzymes and their multi-enzymatic properties can control the level of reactive oxygen species (ROS) in cells or tissues, for example, oxidase (OXD) and peroxidase (POD) activity can be used to generate ROS, while catalase (CAT) or superoxide dismutase (SOD) activity can scavenge ROS. In the case of ovarian cancer, most commonly nanoceria is being investigated, and also when folic acid is combined with nanoceria there are additional advantages like inhibition of beta galactosidase. Nanocarriers are also used to deliver small interfering RNA that are effective in cancer treatment. Studies have shown that iron oxide nanoparticles are actively being used for drug delivery, similarly ferritin carriers are used for the delivery of nanozymes. Hypoxia is a major factor in ovarian cancer, therefore MnO2-based nanozymes are being used as a therapy. For cancer diagnosis and screening, nanozymes are being used in sonodynamic cancer therapy for cancer diagnosis and screening, whereas biomedical imaging and folic acid gold particles are also being used for image guided treatments. Nanozyme biosensors have been developed to detect ovarian cancer. This review article summarizes a detailed insight into breast and ovarian cancers in light of nanozymes-based diagnostic and therapeutic approaches.
Keywords: breast cancer, ovarian cancer, nanoenzymes, diagnosis, treatment
Graphical Abstract:
Introduction
Cancer is one of the leading causes of mortality, and the existing burden is anticipated to increase by the lifestyle issues and risk factors linked with the prognosis of cancer.1 IARC reported that each year there are 14 million new cases and 7.5 million cancer deaths in the world. The incidence ratio of cancer is greater in developed countries as compared to developing countries.2 However, recent studies show that developing countries account for 15 million prevalent cancer cases, 5 million cancer deaths, and 8 million new cancer cases. As a consequence, about 21 million new cases of cancer are expected to occur annually by 2025.3
Breast cancer has been found to be the second most prevalent cancer type after lung cancer and has been ranked fifth as a cause of death. It is more common in females, especially in developing countries.4 Primarily in western countries, the incidence rate of this type of cancer is expected to increase by 30%, mainly due to the use of menopausal hormonal therapy, changes in reproductive patterns, and increased screening in the 1980s and 1990s.5 However, this ratio has decreased or plateaued since the start of the 20th century, which may be due to the sensitization of the people to its risk factor for breast cancer, advanced screening patterns, and increased awareness.6 On the other hand, as compared to western countries, the incidence rate has been continuously increasing in underdeveloped countries because people are unfamiliar with screening patterns and useful information.7
It is a heterogeneous disease and the most frequent malignancy in females. Since the past fifteen years, more treatment options have been developed to take this issue into account, with more focus on treatment de-escalation and biologically directed therapies for reducing the side effects of treatment approaches.8 A driving principle of new treatment approaches is the inherent molecular heterogeneity, but other factors like metastatic patterns or locoregional tumor burden impact are shared and affect therapeutic approaches.9 Breast cancer at an earlier stage (when it has only spread to the axillary lymph nodes or is contained in the breast) is found to be curable. Multimodal therapy improvements have increased the chances of curing breast cancer. By using currently available treatment options, the metastatic (advanced) disease is not curable.10 Advanced breast cancer can be cured by controlling the symptoms with low treatment-associated adverse side effects and improving lifestyle to prolong survival.11
Ovarian cancer is recognized as the foremost common gynecological tumor.12 As of now, there are various considerations distributed in PubMed and NCBI examining the subtle elements of progressed stages of ovarian cancer related to extreme morbidity, which are described within the frame of low survival rates.13 In 2022, 10.6 new cases of ovarian cancer were analyzed in 100,000 ladies yearly. The yearly passing rate was 6.3 per 100,000 females. Non-Hispanic white ladies (12.0 per 100,000) had the most noteworthy predominance of ovarian cancer, taken after by Hispanic ladies (10.3 per 100,000). Ovarian cancer is three times more dangerous than breast cancer, whereas having a lower predominance.14 CA 125 (cancer antigen 125) blood test and transvaginal ultrasound check (TVS) are as of now utilized to analyze ovarian cancer.15 Ovarian cancer is caused by many factors, the most important of which are genetic, environmental, and lifestyle factors. The risk of this condition can be lowered by a number of factors, including pregnancy, breastfeeding, and use of oral contraceptives.14
Ovarian cancer remedies comprise advanced skillful surgical procedures and cytotoxic chemotherapy and radiotherapy. In reality, routine treatment for progressed ovarian cancer is maximal cytoreductive surgery taken after by platinum- and/or taxane-based chemotherapy. After initial treatment, 75% of patients demonstrate a complete clinical and biological response. However, mostly he relapses within 18–24 months. Unfortunately, 5-year survival rates are the result of developing drug resistance, making maintenance therapy less effective. Despite the fact that chemotherapy is highly effective in treating ovarian cancer, drug resistance remains a major obstacle to patient treatment and favorable prognosis. It is widely believed that the physiopathology and molecular science of ovarian cancer improvement can provide individualized cancer treatment. There are contemporary advancements that make use of common organic or atomic qualities at the tumor genesis location.16 Poly-ADP-ribose polymerase inhibitors have been found to make strides in progression-free survival.17
Nanozymes can be utilized in the diagnosis of ovarian cancer through various approaches such as biomarker detection, multiplex detection, non-invasive Imaging, and early detection. Similarly, nanozymes hold promise for the treatment of breast cancer through various therapeutic strategies such as targeted drug delivery photothermal therapy (PTT), radiotherapy enhancement, immunotherapy enhancement, and theranostic treatments. In short, nanozymes offer innovative approaches for both the diagnosis of ovarian cancer and the treatment of breast cancer, with the potential to improve detection accuracy, treatment efficacy, and patient outcomes in these challenging diseases.17,18
Modern treatment supports logical inquiries about the ways to detect the cancer early and about recommending the remedy of nanozymes for cancer treatment and early bio-detection. Nanoparticles are found to specifically impact organic components like autophagy as well as imitate enzymatic capacities shown by superoxide.18 Almost 45.6% of patients with this dangerous sickness survive five years, all due to the lack of early cancer diagnosis.19 The absence of a common and early screening test is encouraging and contributes to delayed discovery. These components are likely to make ovarian cancer worse, as well as breast cancer known as the “silent killer”.20
Nanozymes
Nanozymes are made up of nanomaterials (1–100 nm) that perform enzyme-like activities and mimic the catalytic activities. The term nanozymes and nanoenzymes are used interchangeably. Under physiological conditions, they can catalyze enzymatic reactions just like natural enzymes. According to published research, nanoparticles (NPs) made of Fe3O4 have intrinsic peroxidase (POD)-like properties.21 Now, different types of nanomaterials have been discovered, such as oxidases (OXD), superoxide dismutases (SOD), catalases (CAT), as well as POD-like catalytic type (Table 1). Nowadays, there are about 550 types of nanozymes made up of fifty types of elements that have been found in 350 laboratories in 30 countries. Among these, gold nanoparticles, carbon nanozymes, graphene oxide, CeO2, and iron oxide nanoparticles are widely applied and studied. They can regulate the redox level of cells and catalyze enzymatic reactions22 (Figure 1).
 |
Table 1 Types of nanozymes and their enzymatic activities |
 |
Figure 1 Versatile platforms for cancer diagnosis and therapy. This figure represents different areas for cancer diagnosis and therapy which can be exploited through using nanoenzymes. |
ROS are the by-products that are produced by the processes of oxygen metabolism . An abnormal increase in the level of ROS, which results in oxidative stress, destroys the homeostasis of redox. Oxidative stress is a term referred to as an imbalance between the production of reactive oxygen species (ROS) and the ability of the body to detoxify them or repair the resulting damage. Nanozymes can exhibit different enzymatic reactions.24 The superoxide dismutase and catalase activities of nanozymes, which are involved in important processes of cell protection mechanisms, can regulate the intracellular ROS level.25 Meanwhile, the peroxidase and oxidase potentials of nanozymes induce the production of ROS and induce apoptosis in cancerous cells (Figure 1). Because of easier preparation, low cost, biosafety, high stability, and high catalytic efficiency, nanozymes are now widely used in environmental remediation, especially in relation with biological, medical, and industrial fields.26 Now, different nanozymes-based nano sensors are used for wound healing, bone marrow therapy, cancer therapy, and as antimicrobials.27
Classification of Nanozymes
Nanozymes are of different types on the basis of their functions, including translocases, ligases, isomerases, lyases, hydrolases, transferases, and oxido-reductases. Most of these enzymes have SOD, CAT, OXD, and POD-like activities, and a small number of them can perform these activities along with hydrolases28 (Figure 2).
 |
Figure 2 Classes of nanozymes. This figure shows the classification of nanoenzymes having significance in cancer diagnosis and treatment. |
POD-Like Nanozymes
They can oxidize the substrate by using organic peroxides or hydrogen peroxide. Most of them can produce high-valence by-products by activating H2O2 because of being a ferric heme protein.29,30 They can also abstract electrons from various substrates. Various iron-based nanomaterials mimic the POD-like activity31 (Table 1). It was found that Fe3O4 nanoparticles can catalyze different POD substrates such as o-phenylenediamine (OPD). Other iron-containing nanomaterials, such as Fe3O4 nanoparticles, can mimic the POD, and their iron part is present in the form of hemin, single iron sites, Prussian blue, and iron chalcogenides32 (Figure 2).
A team of researchers has prepared the nanocomposites from Janus γ-Fe2O3/SiO2 (JFSNs) which are more stable at high temperature and pH and act as more stable as compared to horseradish peroxidase (HRP), which is a natural enzyme.33 They exhibit a greater maximal reaction velocity (Vmax) value and a lower value of the Michaelis constant (Km) than HRP. JFSNs produced using the 3,3′,5,5′-Tetramethylbenzidine substrate (TMB) show greater enzymatic activity and higher affinity. Similarly, another type of nanozyme was made by 9-fluorenylmethyloxycarbonyl (Fmoc)-L-histidine (FH) and hemin.34 The morphology and size of this nanozyme can be changed by adjusting the FH and hemin ratio.35
Additionally, nanomaterials containing transition metals such as Ruthenium (Ru), Osmium (Os), Iridium (Ir), Palladium (Pd), Platinum (Pt), Silver (Ag), Gold (Au), Copper (Cu), Tungsten (W), Molybdenum (Mo), Manganese (Mn), Cobalt (Co), Zinc (Zn), and Vanadium (V) can also act as PODs. It was found that V2O5 nanowires can catalyze the oxidative reactions of TMB and 2,2-azino-bis (ABTS) by using H2O2. For the oxidation of ABTS at the expense of H2O2, the Km values were found to be 0.4 and 2.9 μM at pH 4.0, which are smaller than natural enzymes. It indicates that V2O5 nanowires have a high affinity for substrates.36 Four types of V2O5-based nanomaterials were prepared, having different morphologies such as nanospheres, nanoflowers, nanosheets, and nanowires, and mimicking GPx-like activities.37 These activities are dependent on the crystal faces, morphology, and size. Natural enzymes require metal ions for their activities, but these synthetic enzymes do not require other elements for their catalytic activity.38
Single-walled carbon nanotubes (SWCNTs) can produce an oxidized form of TMB through their catalytic activity and can change their colors. This system was used for the diagnosis of single nucleotide polymorphisms (SNPs) without further labelling as the SWCNTs possess unique electronic characteristics that make them excellent contenders for such biosensing applications.39 Similarly, graphene oxide (GO) nanosheets can perform POD activities.40 By focusing on these properties of nanomaterials, GOx and GO nanozymes were built for the detection of glucose. As zero-dimensional carbon nanomaterials, graphene/carbon quantum dots can also function as PODs.41 Recently, it was indicated that graphene quantum dots that can mimic the POD-like activities have higher catalytic activities because of carboxyl and carbonyl groups, which act as binding and catalytic sites.42
Ag2S@Fe2C-DSPE-PEG-iRGD, a nanozyme system based on nanoparticles, was designed by the coating of Ag2S@Fe2C NPs surface with DSPE-PEG-iRGD (Distearoyl phosphoethanolamine-PEG-iRGD peptide). This system indicated the up-regulation of ROS, good fluorescence performance, and intracellular uptake in breast cancer cells (4T1). Moreover, this nanozyme also showed bioimaging effect under in vivo experiments. It was a novel therapeutic strategy for the treatment of breast cancer.43
OXD-Like Nanozymes
They are involved in catalyzing the redox reactions by using molecular oxygen (O2), which will be converted to H2O and H2O2. It was reported that AuNPs can transform glucose into gluconate by performing GOx-like activities44 (Table 1). Now, ultrasmall nanomaterials on the basis of Ir, Pt, Ag, and Cu are used because of their OXD-mimicking properties. Some researchers synthesized gold nanoparticles as catalysts and seeds.45 It was observed that gold nanoparticles with a 13-nm size showed a higher reaction rate for glucose but lower affinity as compared to natural GOx. This outcome is attributed to factors such as increased surface area, size-dependent quantum effects, enhanced mass transport, and conformational changes induced by the nanoparticle surface.46
Similarly, Ir nanoparticles having 2.5 ± 0.5 nm diameter were synthesized, and they catalyzed the TMB oxidation due to the formation of blue product in the presence of oxygen.47 Ir nanoparticles having OXD-like properties can be used for the detection of oxygen. Similarly, GSHOx-like nanozymes were prepared for the generation of hydrogen peroxide at the expense of glutathione.48,49 Cerium oxide has OXD-like catalytic properties, and they are also known as ceria nanoparticles or nanoceria. It was indicated that nanoceria in acidic environment promoted the oxidation of various substrates.50 Their functional properties can be increased by decreasing their size. Organic nano assemblies and inorganic nanomaterials possess OXD-like properties. It was found that phthalocyanine and FH can be used in fabricating photo oxidase-like nanovesicles.51 After the formation of nanovesicles, their self-aggregations were decreased for increasing the photostability and photosensitization. For higher photooxidation of dopamine, the nanovesicles with OXDs can be used.52
CAT-Like Nanozymes
Biological catalysts are present in all living organisms and play a role in the decomposition of H2O2. The natural CATs contain iron-containing heme moieties and show strong bonding with H2O2. Different carbon-based and metal-containing nanomaterials can perform CAT-like activities. The ultrasmall gold nanoclusters loaded with indocyanine were prepared, and they catalyzed the CAT-like activities53 (Figure 2). These nanoclusters showed superior CAT-like properties and substrate affinity.54
Adenosine monophosphate (AMP) and Fe3+ were used for the formation of coordination nanoparticles (CPs) exhibiting CAT-like properties55 (Table 1). The Fe3+/AMP CPs, compared to natural CAT, had a greater kcat/Km ratio and a lower Km value, which showed their strong catalytic efficiency and higher affinity for the degradation of hydrogen peroxide. In an experiment, it was observed that graphene oxide quantum dots produce gas bubbles after incubation with hydrogen peroxide, which showed their CAT-like properties.56,57 Moreover, a study indicated that 100 µg L−1 graphene oxide quantum dots can perform the CAT-like properties, which is the same as 4 UL−1 natural enzyme.58
SOD-Like Nanozymes
They can help to dismutate the superoxide radical (O2) into H2O2 and O2, which act as defense mechanisms. Naturally occurring SODs are of three types based on their metal cofactors and protein folds: the Ni type, Fe and Mn type, and Cu/Zn type. Nanomaterials having these metal elements can perform SOD-like activities59 (Table 1). In a study, NiO nanoflowers were used for the generation of O2 by scavenging O2− which showed high SOD-like activities.60 It was found that ceria nanoparticles having higher ratio of Ce3+/Ce4+ showed these properties61,62 (Figure 2).
Factors Affecting Nanozymes Activity
The functions and properties of a nanozyme are regulated by some factors: surface modification, structure, size, and shape.63 In this article, some factors by which the catalytic functions of nanozymes are affected have been discussed. The discussed factors include morphology, size, composition, surface, modification, etc.
Morphology
The catalytic functions of nanozymes are regulated by their Morphology. For example, it was found that the enzymatic activities of LaNiO3, CoFe2O4, MnO2, Co3O4, and Fe3O4 are regulated by their morphology.64 VO2 nanofibers showed high POD-like activities on the basis of large surface area as compared to VO2 nanosheets (NSs) and nanorods (Table 2). Additionally, Mn3O4 nanoflowers have higher enzymatic activities as compared to polyhedrons, hexagonal plates, flakes, and cube-shaped nanozymes because of their large pore size and surface area.65
 |
Table 2 Different regulation strategies for the activities of nanozymes |
Size
Another factor that controls the function of nanozymes is their Size.82 Usually, small-sized nanoparticles exhibit high catalytic activities.83 Small sizes of Fe3O4NPs were found to have high POD-like activities. Similarly, another group of researchers demonstrated that by tuning the size of cerium oxide nanoparticles, their function could be increased or decreased84 (Table 2).
Composition
The Composition of nanozymes also affect their properties. Nanoceria SOD activity is dependent on the nanostructure of the composition.85 Additionally, the combination of more than nanoparticles also enhances the catalytic functions.86 If the active core of the nanomaterials is less etched, the catalytic functions can be increased. The production of Pt hollow nano dendrites with a high index and more active sites showed higher PODs87 (Table 2).
Surface Modification
Surface modification of nanozymes is influenced by covalently immobilizing functional groups and electrostatic adsorption. Moreover, the catalytic functions of nanozymes can also be regulated by the increasing number of active sites in nanozymes. Coating nanozymes can also improve their catalytic functions. Similarly, coating the Fe2O3NPs with Prussian blue can improve the POD-like activities of nanozymes. If the surface charge of nanovesicles is changed from positive to negative, the binding to the substrate is also increased88 (Table 2).
pH and Temperature
Another important factor that controls the catalytic functions of nanozymes is their pH. Some nanozymes showed different catalytic functions upon changing the pH values.35 For example, lowering the pH to 5.3 increases the POD activities of -ZrO2 nanoparticles. It was found that the catalytic functions of iron oxide nanoflowers increased by changing the temperature from 15 to 65 °C as compared to those of HRP under these conditions89 (Table 2).
Nanozyme-Based Early Diagnosis
Nanozymes as multifunctional or bifunctional molecules not only possess enzymatic reactions but also chemical or physical properties of nanomaterials, eg, photothermal and magnetic activities90 (Table 3). Nanozymes are favored because of their low cost, simple preparation, easy modification, and high stability. They are used in disease diagnosis because of their multienzyme activities.91
 |
Table 3 Diagnosis application of different diseases by nanozymes with the particular activity |
Flower-Like Nanozymes
To diagnose the breast cancer biomarkers, the development of highly selective and sensitive approaches is required. An aptasensor was developed to detect breast cancer, and this sensor was made by combining horseradish peroxidase/nanozymes as signal nanoprobes and tetrahedral DNA nanostructures (TDNs) aptamer as a detection probe. It was found that this aptasensor holds a huge potential to detect breast cancer.92
Iridium/Ruthenium Nanozyme
An Ir-Ru nanoenzyme reactor was developed which holds the potential to treat breast cancer by oxidation therapy and starvation therapy. The GOx and Ir-Ru NPs were coated by polyethylene glycol for the construction of multifunctional complex IrRu-GOx@PEG NPs. This complex degrades the nutrient source of cancer cells or induces the apoptosis of tumor cells, reducing the hypoxic problem. This study demonstrated that nanoenzyme systems can be used with oxidative or starvation therapy to inhibit the growth of tumor cells93 (Table 3).
Copper (II) Oxide Nanozyme
A cytosensor based on CuO nanozymes was designed for the quantification of MCF-7 breast cancer cells. This sensor was made by using reduced gold nanoparticles as a supporting material with CuO nanozyme. CuO increased the detection limit of this sensor and has good potential for the selective detection. This approach is combined with antibodies or cell-targeting aptamers, for sensing of other types of cancer cells.92
Platinum Nanoparticles/Graphene Oxide (PtNPs/GO)
It was indicated that porous platinum nanoparticles can be produced in laboratory on PtNPs/GO. In the presence of hydrogen peroxide, PtNPs or GO can catalyze peroxide reactions due to their peroxidase potential, which results in TMB color reaction. Folic acid (FA) was used to modify the PtNPs and GO, which specifically targeted tumor cells because of their higher expression of folic acid receptors. To detect tumor cells, FA-PtNPs/GO was used as a signal transducer.26
Graphitic Carbonitride Nanosheets (g-C3N4NSs)
Some researchers detected breast cancer cells using graphite carbonitride nanosheets (g-C3N4NSs). On the (g-C3N4NSs), the adsorption of ssDNA can promote the catalytic activity of the nanosheets. As compared to unmodified NSs, the modified structures can speed up hydrogen peroxide reactions at a faster rate in TMB oxidation mediated by the hybrid of ssDNA-NSs. The higher catalytic activity of this hybrid mediates the colorimetric detection of exosomes by using a suitable exosome surface marker such as CD 63 while constructing the hybrid. The sensor then measures the expression of a biomarker in control and breast/ovarian cancer cell line.94
M-HFn (Magnetic Heavy chain Ferritin Nanozymes)
They are used to target or visualize the cancer cells without any contrast agents. Ferritin proteins are involved in iron storage for anti-oxidation and iron homeostasis.
Iron Oxide-Based Nanozymes
These nanozymes contain human heavy-chain ferritin (HFn), which is packed in a shell and binds to the cancer cells having higher expression of transferrin receptor 1 (TfR1). The iron oxide-based nanozymes, both Fe2O3 and Fe3O4, can catalyze peroxidase substrate oxidation to detect cancerous tissues by producing a chromogenic reaction. This detection approach helps in the diagnosis of cancer cells with 95% specificity and 98% sensitivity. Moreover, this approach is economic, rapid, and simple. For tumor detection, it can simplify the conventional immunohistochemical method and reduce the test time from 5 to 1 hour and improve the effectiveness of the diagnostic test95 (Table 3).
Graphene Quantum Dot Nanozymes (GQDzymes)
In the presence of hydrogen peroxide, graphene quantum dot nanozymes (GQDzymes) have peroxidase-like activities that can oxidize the 2,20-azino-bis (3-ethylbenzothiazoline-6-sulfonic acid) (ABTS). After oxidation, ABTS has a near-infrared (NIR) absorbance.96 A folic acid-modified nanozyme erythrocyte membrane-coated GQDzyme/ABTS was created, which can directly target cancer cells. Similarly, gold nanoclusters (very small) can be used as a probe for diagnosing tumor-enriched cells or tissues.97
A protease nanosensor was developed by using gold nanoparticles that can perform multiple functions and have peroxidase-like activity. They can detect the disease very quickly and respond to the disease by producing colorimetric signal readings. Researchers confirmed the catalytic potential of these nanozymes in the urine of a cancerous model. When compared to a healthy mouse, a cancerous mouse showed a 13-fold increase in signal. Through renal and hepatic excretion, nanosensors were excreted within one month and showed no toxic effects. Due to the low sensitivity of nanozymes, their use in magnetic resonance imaging (MRI) is challenged.98
The inorganic components (manganese and iron) were used for functional magnetic resonance imaging by producing nanogels through an in-situ reduction process and self-assembly.99 A nanogel-based probe with two enzymes (SOD/biotin-CAT/acryl/SPIO@GCS or SGC) was made for detecting the dual-mode pathologic response by magnetic resonance imaging and ultrasound (US) imaging. The nanozyme was made up of superparamagnetic iron oxide nanoparticles with superoxide dismutase and catalase activities and chitosan gel made by polysaccharide cationic polymer glycols. The dual-imaging properties of the nanozymes were evaluated in vitro and in vivo. The higher response to the tumor region can improve the dual function of this enzyme for more efficient and sensitive tumor imaging100 (Table 3).
Nanozymes in Cancer Therapy
Current treatment therapies have a lot of adverse side effects and a poor prognosis (Figure 3). Nanozymes can perform their activities as natural enzymes and are used for treating cancer. They can target cancer cells by targeting peptides and causing enhanced permeability and retention (EPR).101,102 They kill tumor cells in two ways: first, by increasing ROS in the body through peroxidase and oxidase potentials, which is a direct attack on tumor cells; and second, by increasing SOD and catalase potential (indirect killing) by decreasing tumor microenvironment hypoxia, which is aided by chemo, sound, or light therapy.103
 |
Figure 3 Destruction of tumor cells through N-PCNS. |
Nanozymes as Potential Treatments for Breast Cancer
Nanozymes can directly or indirectly kill breast cancer cells by enhancing reactive oxygen species through peroxidase and oxidase activities. Around the tumor cells, a large amount of H2O2 accumulates, and the peroxidase enzyme converts it into cytotoxic-free radicals. Fanet et al have produced nanozymes by using nitrogen-doped porous carbon nanospheres. They further regulated the ROS.104 New carbon nitrogen nanozymes under acidic environment can catalyze the formation of reactive oxygen radicals by catalyzing hydrogen and oxygen peroxides. The activities of superoxide dismutase and catalase scavenge-free radicals in a neutral environment105 are shown in Figure 4.
 |
Figure 4 Biochemical applications of nanoceria. |
Ferritin nanoparticles modified with carbon nitrogen can directly target cancer cells by being present in the lysosomes while catalyzing hydrogen and oxygen peroxide and producing ROS to specifically kill the cancer cells. Animal trials have shown that this nanozyme can control the growth of tumor cells by enhancing ROS106 (Figure 3). Similarly, the B7-H4 combinational therapy has also been proven to be suppressive for breast cancer, as well as large amounts of reactive oxygen species can be produced by ascorbic acid, which in turn affects the normal redox state of cancer cells. But when they are applied in vivo, the tolerable doses of ascorbic acid were found to be less effective.107
Fe3O4@C Nanoparticles (NPs)
A peroxidase-like composite nanoparticle was created by using ascorbic acid. Researchers developed Fe3O4@C nanoparticles and used folic acid for their modification. The Fe3O4@C NPs carbon shell is graphitized with carbon, which helped to catalyze the electron transfer process by using H2O2 and resulted in the production of ROS. These nanoparticles showed peroxidase-like catalytic potential, receptor-binding specificity, and magnetic responsiveness, which in turn induced ascorbic acid-mediated oxidative stress in tumor cells.105
Superparamagnetic Iron Oxide Nanoparticles (SPIONs)
SPIONs are also studied because of their peroxidase potential.108 In the study, SPIONs were used to produce ROS and combined it with a novel anti-cancer drug (b-lapachone) to increase their potential for inducing 10-fold more oxidative stress in breast tumor cells. A tumor microenvironment favors the chemical and physical conditions for the therapy.106
GOD-Fe3O4@DMSN (GFD NCs)
The GOD-Fe3O4@DMSN (GFD NCs) were synthesized by incorporating glucose oxidase (GOD) and ultra-small Fe3O4 nanoparticles into large-pore dendritic and degradable silica nanoparticles. These nanozymes, when transported to the tumor site, resulted in the apoptosis of the cancer cells by transforming into hydroxyl radicals with greater toxicity and efficiency.109
Nanozymes for Reducing Hypoxia with PtFe@Fe3O4 Nanozyme
The nutrient consumption of a tumor is reduced by the catalase activity of enzymes, which can reduce hypoxia. They can promote the apoptosis of cancerous cells and improve the efficiency of photodynamic therapy, sonodynamic therapy, and radiotherapy.110 In a tumor microenvironment, the composition of hydrogen peroxide and acid contents is higher as compared to normal cells. Tumor hypoxia can cause distant metastases and increase the tumor resistance to chemotherapy. Li et al developed the PtFe@Fe3O4 nanozyme, which can convert hydrogen peroxide to hydroxyl and oxygen radicals, effectively kill cancerous cells, and overcome the hypoxic environment.111
Prussian Blue Nanoparticles (PHPBNs)
A nanosystem was created by combining photothermal therapy and tumor starvation. Glucose oxidase was added to the porous hollow PHPBNs, and they were coated with hyaluronic acid, which was then specifically bound to the CD 44-overexpressing cancer cells for targeting cancer cells. The photothermal properties of PHPBNs in the hypoxic tumor microenvironment can catalyze the breakdown of hydrogen peroxide and kill the tumor cells.112
Another new method is photodynamic therapy for treating cancers with laser activation and photosensitive drugs. Tumor sites are irritated with laser-specific wavelengths, which stimulate photosensitive drugs to start accumulating at the tumor sites and trigger photochemical reactions to disrupt the cancer (Figure 4). The effectiveness of photodynamic therapy is limited by the presence of a hypoxic microenvironment at the tumor site. In the tumor sites, the oxygen content is increased by nanozymes through catalase activity.113
Manganese Dioxide (MnO2) Nanoparticles
To increase the effect of cancer-specific photodynamic therapy and regulate the tumor hypoxic microenvironment, some researchers used MnO2 nanoparticles in catalyzing endogenous hydrogen peroxide to oxygen radicals.114 It was indicated that a universal and simple technique to increase the PDT is by coating the nanozymes with a photosensitizer-integrated metal-organic framework (MOF). Platinum nanoparticles after fixing on MOF destroy the cancer cells due to catalase activity and the formation of oxygen radicals in the hypoxic tumor microenvironment.
AuNCs-NH2 (Amino Terminal PAMAM Dendritic-Coated Gold Particles)
Furthermore, Liu et al demonstrated that AuNCs-NH2 can effectively produce oxygen radicals via catalase activities for cancer treatment.56,57
Nanozymes as Potential Treatments for Ovarian Cancer
Oxidative stress is arguably important as it is involved in many intractable clinical diseases such as cancer, diabetes and cardiovascular disease. Baseline levels of ROS are already high in cancer cells, and the oxidative properties of CNPs (cerium oxide-based nanoparticles) at acidic pH led to additional increases in ROS above threshold levels that trigger cell death. While there are a number of redox-active nanomaterials that can be used to fight cancer, CNP can regenerate, reduce elevated ROS levels without affecting baseline levels in healthy cells, and reduce pro-oxidants in cancer cells. It is special because it selectively activates and ultimately causes ROS-induced cell death of cancer cells.115
Cerium oxide nanomaterials (also called nanoceria) as well as curcumin nanoparticles are known for their interesting characteristics (ie, the closeness of blended valence states of Ce3+ and Ce4+ and exceedingly versatile grid oxygen), and cerium oxide nanoparticles have been used broadly as amazingly compelling catalysts. They too have been completely explored for their potential to imitate the capacities of characteristic proteins.77 It was assumed that nanoceria might shield tumor cells from radiation-induced injury but not ordinary cells. Since that point, various experiments have illustrated that nanoceria may mirror different proteins, counting catalase, oxidase, peroxidase, and phosphatase.116,117 These nanozymes would avoid the improvement of myofibroblasts, subsequently avoiding the metastatic spread of tumor cells.118 Ovarian tumor development may be restrained by nanoceria through an anti-angiogenic instrument.119
Nanoceria can serve as useful operators for ovarian cancer cells both in vitro and in vivo. Nanoceria could reduce cell motility and aggression without altering cell proliferation by limiting ROS assembly and proliferation induced by vascular endothelial development factors. Furthermore, it was later shown that folate-conjugated nanoceria (FA-CeO2 at 24.3+) decreased ovarian cancer cell expansion (due to higher cell anabolicity) and increased ROS age. Both studies showed that nanoceria, despite its main or contrasting antioxidant properties, was associated with a striking reduction in tumor development and narrowing of angiogenesis in nude mice with ovarian cancer. Furthermore, they showed that expansion of FA-CeO2 to cisplatin significantly reduced tumor burden compared to the group that received cisplatin alone.120,121
In vitro nanoceria nanozymes functioned by transforming developmental factor-mediated cell migration and attack on SKOV-3 cells, significantly reducing cellular ROS in A2780 cells, without affecting the regenerative capacity of each cell. Nanoceria nanozymes appear to reduce VEGF165-induced proliferation, capillary assembly, and VEGFR2 staging in HUVEC cells. Nanoceria nanozymes (0.1 mg/kg body weight) were given intraperitoneally to nude mice in order to cure A2780 ovarian cancer cells in vivo, in which the angiogenesis and carcinogenesis of ovarian cancer in rats were both decreased by nanoceria.121
The effects of nanoceria nanozymes on ovarian and colon cancer cells were closely linked to those effects. The patient’s ROS levels in the intracellular space were reduced by 7 nm and 94 nm nanoceria nanozymes in both cell models. Moreover, larger nanoceria had a stronger ROS scavenging effect than smaller nanoceria in these cell lines.122,123
Nanoceria Utilized with Folic Acid for Therapy
Folate may be a promising alternative for focused anticancer treatment since cancer cells are intensely subordinate to it for generation and indeed make them possess receptors that are not overexpressed in noncancerous cells. Nanoceria has antioxidant and antiangiogenic characteristics that result in a strong anticancer impact on ovarian cancer.124 By taking use of the specific expression of folic acid receptors in cancer and physical cells, conjugating nanoceria with folic acid seems to have enhanced the restorative effect of nanoceria on ovarian cancer. Because of folic acid conjugation with nanoceria, which has a far higher adaption to cells, it is much simpler for nanoceria to specifically target cancer cells. Tumour angiogenesis, which is essential for the expanding tumour to receive oxygen and other nutrients and is either characterised by excessive production of pro-angiogenic signals or by a requirement for angiogenesis inhibitors, is essential.125,126 In this regard, many novel medicines have been licensed by the US Nourishment and Sedate Organization for ovarian cancer since 2004.126 Tumor angiogenesis inhibition has recently emerged as a curative anticancer technique. In our earlier research, it was discovered that nanoceria had considerable antiangiogenic effects both in vitro and in vivo that are independent of VEGF production. This was hypothesised to be due to endothelial cell focus, which inhibits the growth of inactive blood vessels. As evidenced by the reduced expression of CD 31, a marker for endothelial cells, in the nanoceria-folic acid and nanoceria folic acid/cisplatin treated groups compared to the untreated group, the thickness of the microvessels in each group was examined. In any event, the CD 31 thickness of the NCe-FA and cisplatin combination group and the cisplatin alone group was equivalent, despite the fact that the NCe-FA and cisplatin treatment resulted in a decreased tumour burden score. The vessels had the same thickness. An EMT marker called vimentin was communicated less when NCe-FA was present, perhaps limiting the spread of ovarian malignancies127 (Table 4).
 |
Table 4 Properties of Nanoceria |
Nanocarrier-Delivered Small Interfering RNA
Ovarian cancer has an overexpressed form of hyaluronic acid (HA), which is a ligand for CD 44 and is thought to be a potential molecular target. Self-assembling HA nanoparticles (HA-PEI/HA-PEG) effectively deliver MDR1 siRNA to MDR ovarian cancer cells and inhibit P-gp expression.129 In a mouse model of multidrug-resistant ovarian cancer, P-gp expression was significantly decreased following treatment of paclitaxel and HA-PEI/HA-PEG/MDR1 siRNA nanoparticles. Guo et al created the amphipathic cationic polypeptide LAH4-L1. It uses electrostatic interactions to bind MDR1 siRNA and create LAH4-L1/siRNA complexes (LCSs) as a means of delivering genes. LSC lowered P-gp by 85% and silenced the MDR1 gene in SKOV-3 cells with an effectiveness of 87.3%. More importantly, combining LSC with chemotherapeutic agents reduced SKOV-3 cell proliferation by 82.9%.130
Drugs used in chemotherapy can make tumour cells undergo apoptosis. Drug resistance can be brought on by faulty apoptotic pathways or stronger anti-apoptotic defenses. The gene Bcl-2 (B-cell lymphoma 2), for instance, regulates programmed cell death.131 In many organs, Bcl-2 controls cell apoptosis, according to a different study. Notably, Bcl-2 is overexpressed in ovarian cancer, which is directly related to tumours that are resistant to chemotherapy. PLGA nanoparticles were loaded with MDR1 and Bcl-2 siRNAs as a dual RNAi delivery method.131
Peroxidase Activity of Iron Oxide and Ceria NPs
The primary illustrations of nanoparticle chemical mirrors were iron oxide and nanoceria nanoparticles inherent peroxidase action.61,62 The breakdown of peroxide into water and atomic oxygen is catalyzed by normal peroxidases with vanadium or iron oxide. A strategy was developed for concurrently focusing on and picturing tumors based on the inborn peroxidase-like movement of iron oxide NPs.95
Iron oxide nanoparticles (NPs) can be identified by human overwhelming chain ferritin (HFn). The target of the specific official of HFn to this receptor is the transferrin receptor 1 (TfR 1), which is overexpressed in malignant cells. The imaging is made possible by the peroxidase action of iron oxide NP, which causes a colour response with peroxidase substrates close to H2O2. The magnetoferritin-NP combination has a notable affectability (98%) and specificity (95%) for attaching to tumour cells when compared to antibody-based approaches. The magnetoferritin-NP complex may offer an effective alternative to conventional cancer and tumour treatment.95
Under physiological conditions, peroxidase-active iron oxide nanoparticles (NPs) deliver oxygen radicals close to H2O2 based on the Fenton or Haber-Weiss reaction.81,132 Germs and cancerous cells are destroyed by oxidative stress, which is brought on by an increase in ROS. In vivo analyses of ROS generation and in vitro experiments with microorganisms were used to demonstrate the peroxidase-like action of magnetite nanoparticles81 (Figure 5).
 |
Figure 5 Schematic representation of the antioxidant activity of nanoceria (middle), by analogy with native superoxide dismutase (SOD) and catalase (CAT), hypotheses were made for this mechanism. |
Escherichia coli (E. coli) and a HeLa cell show were utilized to report on the antibacterial impacts and in vitro tumor cell investigations. Both investigations’ discoveries are steady with the chosen component and rising ROS levels. Within the bacterium examination and within the investigation of person cells, H2O2 and magnetite NPs did not display solid cytotoxic impacts. Extra inquiry about imaging and treatment of tumors may need to be illustrated by further inquiry; meanwhile, the take-up of MNPs by cells is based on the EPR impact. Apoptosis is based on intracellular ROS generation, and the discovery of tumor tissues is made conceivable by T2-weighted MR imaging133 (Figure 6).
IONP Drug Delivery Without a Mechanism of Drug Release
Due to their biocompatibility and the various ways in which their therapeutic efficacy can be activated, iron oxide nanoparticles (IONPs) are at the forefront of the most extensively studied nanomaterials. Whereas chemotherapy medications are delivered to tumors utilizing IONPs (press oxide nanoparticles), they have the taking after benefits over being infused intravenously: (i) the capacity to limit IONPs and, subsequently, the sedate conjugated to IONP, utilizing MRI as an illustration; (ii) the increment in sedate aggregation within the tumor; (iii) for occurrence, doxorubicin (DOX)-containing IONPs driven to a better concentration of DOX in tumor cells when compared with free DOX treatment in an ovarian cancer show.134
When chemicals are bound to IONPs, they produce ROS (as demonstrated by cisplatin bound to IONPs), where nicotinamide adenine activates dinucleotide phosphate oxidase (NOX), or when IONPs dissolve into Fe2+ and/or Fe3+. Dioxygen (O2) is transformed into superoxide radicals and HO. Additionally, ROS have been demonstrated to have minimal systemic effects while causing oxidative damage to lipids, proteins, and DNA at tumour locations.135,136
Ferritins as Carriers for the Delivery of Nanozymes
Ferritin with artificial nano-CeO2 is an unused nano-complex development strategy (AFt-CeO2). In their inquiry about the organization of 4.5 nm nanoceria particles, they are effectively separated and after that they are modified into the apoferritin depression. The apoferritin embodiment is seen to impact and subsequently changes the nanoceria’s cellular retention course, increments biocompatibility, as well as controls electron area at the nanoparticle’s surface, which upgrades ROS-scavenging movement137 (Figure 5).
Peroxidase oxidation can be quickened by nanoparticles. Nanoparticles work by acting as a catalyst within the oxidation of peroxidase substrates within the nearness of hydrogen peroxide to create a color response comparable to that of common peroxidases. Besides, human transferrin TfR1 was found to be an endocytosing cell-surface receptor for HFn. TfR1 can mediate the HFn to TfR1-positive cancer cells due to its liking for the compound. In reality, HFn can perceive all sorts of cancer cells, counting SKOV-3 ovarian cancer cells.138
MnO2-Based Nanozymes in Hypoxia Relief
It is well known that tumor hypoxia is a significant obstacle to cancer therapy. Tumor cells undergo both genetic and proteomic changes in a persistent hypoxic environment. Hypoxia-mediated changes promote tumor growth, invasion and metastasis and help tumor cells adapt and survive in hostile environments. Clinical evidence from numerous independent reviews associates hypoxia with poor prognosis in various types of tumors, including ovarian cancer.139 Nanozymes are nanomaterials with enzyme-like catalytic properties. Due to their characteristic properties, artificial synthesis, excellent stability and resilience, these engineered enzymes have been the subject of many recent studies. The catalytic ability of some nanozymes has been used to breach the hypoxic barrier in cancer therapy. Manganese oxide (MnO2) nanoparticles were the first nanozymes used for in situ O2 generation in hypoxic tumor microenvironments. Similar to the enzyme catalase, MnO2 NP catalyzes the decomposition of H2O2 to produce O2 at physiological pH.140 An entirely new approach to tumor oxygenation is the on-site generation of O2 by enzymes (catalase) or catalytic nanomaterials (nanozymes). Novel nanomaterials that effectively alleviate hypoxia have beneficial effects on the therapeutic response to cancer (Figure 7).
 |
Figure 7 AI representation of the process of using carriers for the delivery of nanozymes. |
A few nanozymes’ catalytic capacities have been utilized in cancer treatment to break over the hypoxic obstruction. The first nanozyme is in situ O2 arrangement of manganese oxide (MnO2) nanoparticles within the hypoxic tumor microenvironment. Comparative to the catalase enzyme, the MnO2 NPs catalyze the breakdown of H2O2 to make O2 at physiological pH.141 The catalytic action of MnO2 NPs shows its beneficial properties within the shape of three diverse activities: corrupting endogenous H202 which in turn diminishes the likelihood of ROS resultant harm, generation of oxygen in reaction to a hypoxic environment, and direction of pH by utilization of protons which successfully diminishes acidosis.
Sonodynamic Cancer Therapy
Sonodynamic treatment (SDT), a promising non-invasive helpful approach, has pulled in an expanding sum of intrigue in later a long time. Sonosensitizers are its particular chemical operators, and they produced deadly responsive oxygen species (ROS) for oncotherapy when enacted by low-intensity US. SDT offers various exceptional prospects and points of interest over phototherapeutic approaches, counting more profound entrance profundity, nonappearance of phototoxicity, and less side impacts (Figure 8).
 |
Figure 8 Graphical representation of the mechanism involved in SDT. |
The generated ADV phenomenon has been shown to disrupt nearby vasculature during ultrasound (US) irradiation, reducing resistance to drug diffusion and allowing nano-sensitizers to penetrate deep into internal tissues. FA-H@ND supported by US irradiation generated too much ROS, resulting in higher SDT efficiency. Additional analysis also showed a high rate of suppression of ovarian tumors in vivo. Together, these US-activated nanodroplets have created a new paradigm for effective SDT through targeted delivery and complete intratumoral penetration of nano-sensitizers. Vectors made from endogenous cells are considered to be more sophisticated delivery vehicles than nanoliposomes due to their superior biocompatibility and innate ability to avoid uptake by the reticuloendothelial system (RES). It is a nano-sensitizer that penetrates deep into tumors. Vectors made from endogenous cells are considered to be more sophisticated delivery vehicles than nanoliposomes due to their superior biocompatibility and innate ability to avoid uptake by the reticuloendothelial system (RES)142 (Figure 8).
There are efficient methods other than nanocarrier encapsulation-assisted delivery of organic small-molecule acoustic sensitizers to malignant tumors. Delivery of small organic acoustic sensitizers to tumors has also been facilitated by the introduction of self-assembly techniques. For improved SDT, Zheng et al described self-assembled hypocrellin-derived nanoparticles (APHB NPs) have been described. APHB-NPs thus prepared are said to have good biocompatibility, increased tumor accumulation, increased ROS generation and suitable biodegradation rate. These advantages, together with a significant reduction in tumor growth in vivo, clearly supported the idea that assembled APHB-NPs would be excellent SDT drugs.143
Folic Acid Gold Nanoclusters Used in Diagnosis
Bovine serum egg white-based gold nanoclusters (BSA-AuNCs) emit flexible photoluminescence in the initial natural window. Normally estimated to be 2–3 nm in length, the protein polymerized-chains doped with AuNCs within the as-synthesized BSA-AuNCs operators exhibit important properties such as strong photostability, temperature dependence, and excitation-induced photoluminescence. It is discovered that the photostable BSA-AuNCs were functionalized with folic acid in order to actively target NIH: OVCAR-3 human ovarian cancer cells toward bioimaging applications (FA-BSA-AuNCs). After confirming their biocompatibility up to a concentration of 40 mg/mL, routine wide-field epi-fluorescence microscopy was used to validate the increased cellular take-up and recoloring capacity of FA-BSA-AuNCs compared to the BSA-AuNCs. Confocal fluorescence lifetime imaging microscopy (FLIM) was used to monitor the intracellular localization. Due to their advantageous inherent photoluminescent properties, the orchestrated FA-BSA-AuNCs offer impressive potential for coordinated employment in cellular imaging as effective differentiation specialists towards early cancer conclusion and image-guided treatment of cancer.144
Nanozymes as a β-Galactosidase Inhibitor
One of the normal lysosomal glycosidases, -galactosidase (-gal), is believed to be a critical biomarker that is overexpressed in early ovarian cancer cells. Galactosidase (-Gal), a common proteolytic chemical similar to ChT, is essential for catalyzing the hydrolysis of lactose to galactose. Since overexpression of -Gal is typically associated with the development of vital ovarian cancer and cell maturation, inhibitors of -Gal have been produced for use in the clinical conclusion of a variety of disarrangements.137,145
Given the assortment of chemical inhibitors, we have seen an advancement of novel nanoparticle inhibitors with unordinary shapes later years.146 The biocatalytic inhibitory actions of these new inhibitor classes are strongly influenced by shape impacts because of their altered geometries. Previous studies have demonstrated ZnO NPs’ potential for shape direction in the presence of peroxidase.146
Three different types of zinc oxide nanoparticles (ZnO NPs) with various geometries are hexagonal nanopyramids, nanoplates, and nanospheres, characterized by modification of the shape and surface chemistry. The inhibitory effects of the various ZnO NPs on the catalytic activity of -Gal were then methodically compared. Protein mobility gradually decreased as the concentrations of nanoplates and nanopyramids increased but was unaffected by all concentrations of nanospheres.147,148 Furthermore, in comparison to nanoplates, ZnO nanopyramids’ more refined apexes and edges created a more noteworthy degree of geometric coordination with the chemical surface encompassing the dynamic center, driving to the most noteworthy inhibitory impacts. In this manner, atom shape-dependent inhibitory conduct, in expansion to hydrogen bonds and van der Waals forces, is what causes the substrate’s binding strength to the active site to be decreased.
Nanozyme Biosensors Used to Detect Breast Cancer and Ovarian Cancer
When it comes to cancer organizing and conclusion, finding specific miRNAs connected to the illness is straightforward. For occurrence, enzyme biosensors can presently distinguish miR-21, a conceivable biomarker for vertebral cancer, ovarian cancer, and other cancers like breast cancer. Based on a lock exponential rolling circle enhancement (P-ERCA) test and CoFe2O4 attractive nanoparticles, an ultrasensitive electrochemical biosensor for miR-21 discovery was made (CoFe2O4 MNPs).29,30 This test is a latch test characterized with a hybridization arrangement to miRNA and a scratching target location for the endonuclease, making it an exceedingly delicate and particular intensification approach with a location restrain as much as the zeptomole level. Nan Yu and partners utilized this technique to identify miR-21 with a moo location restrain of 0.3 fM and a huge energetic run of 1 fM to 2 nM.149,150
Nanoenzymes in Biomedical Imaging
Biomedical imaging and cancer treatment frequently use nanomaterials like nanoparticles, nanozymes, nanorods, nanospheres, nano shells, and nano stars. Among other things, they serve as contrast agents, photothermal agents, photoacoustic agents, radiation dosage enhancers, and drug delivery agents. Nanomaterials are increasingly being employed in a variety of sectors, including functional imaging, nanofabrication integration, cancer therapy, and synergistic combination platforms, thanks to recent advancements in nanotechnology.151–153 As nanozymes to promote the generation of OH for intracellular oxidative tumor damage by H2O2 present in cancer cells, small AuNPs are preferred over large ones due to their enhanced catalytic activity and the facility of intracellular delivery compared to that of larger AuNPs.109
According to in vivo and in vitro studies, nanoprobes showed excellent tumor-targeting efficacy, long-term tumor retention, and good therapeutic efficacy.154,155 For PDT and PTT, singlet oxygen and photothermal effects can be generated. Due to its small size (60 nm) and surface PEGylation, it accumulates extensively in tumors. All these properties make it potentially usable in image-guided PDT/PTT.107,148,156
Conclusion and Future Perspectives
Nanozymes are diverse in classification and are inspired by nature and have various benefits as well as the factors that are used for the diagnosis and treatment of different diseases. Various techniques are being tested and revalidated to diagnose the breast and ovarian cancers early, leading to the positive prospect of their treatment, however many of these methods are still in experimental stages and are not routinely used for treating patients. Our review concluded that there are many disadvantages, which are fortunately outnumbered by the advantages of using nanozymes. Nanozymes, on the basis of their oxidase, catalase, and peroxidase activities, can be used to diagnose cancer. Depending on these activities, they can also be used to treat cancer. They are the artificial enzymes that mimic natural enzymes and have diverse functions, excellent designability, and strong stability. The knowledge gathered and analyzed in this review is limited because of the lack of research and initiative in nanoenzymes to treat ovarian and breast cancer. Having gone through multiple articles, the majority of selected articles were then further excluded based on our criteria of inclusion criteria which required an association with ovarian cancer, despite its initial understanding. Studies were thoroughly analyzed to ensure that there was an emphasis on nanozymes in comparison to nanoparticles and enzymes which are being used independently for treatment. In the future, it is expected that they can be applied in the medical field and replace natural enzymes. On the other hand, there are some issues that should be resolved: their catalytic efficiency is not up to the level of naturally occurring enzymes, and they have redox activities that are less widely used. The toxicity of nanomaterials has limited their applications, which act as both opportunities and challenges for nanozymes.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (No. NRF.2021R1F1A1062849).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tran KB, Lang JJ, Compton K, et al. The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10352):563–591.
2. Momenimovahed Z, Salehiniya H. Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer. 2019;11:151–164. doi:10.2147/BCTT.S176070
3. Richters A, Aben KKH, Kiemeney LALM. The global burden of urinary bladder cancer: an update. World J Urol. 2020;38(8):1895–1904. doi:10.1007/s00345-019-02984-4
4. Giaquinto AN, Sung H, Miller KD, et al. Breast cancer statistics, 2022. CA Cancer J Clin. 2022;72(6):524–541. doi:10.3322/caac.21754
5. Lee A, Mavaddat N, Wilcox AN, et al. Boadicea: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet Med. 2019;21(8):1708–1718. doi:10.1038/s41436-018-0406-9
6. Fahad Ullah M. Breast cancer: current perspectives on the disease status. In: Breast Cancer Metastasis and Drug Resistance. Springer; 2019:51–64.
7. McKinney SM, Sieniek M, Godbole V, et al. international evaluation of an AI system for breast cancer screening. Nature. 2020;577(7788):89–94. doi:10.1038/s41586-019-1799-6
8. Ezzati M, Yousefi B, Velaei K, Safa A. A review on anti-cancer properties of quercetin in breast cancer. Life Sci. 2020;248:117463. doi:10.1016/j.lfs.2020.117463
9. Yin L, Duan JJ, Bian XW, Yu SC. Triple-negative breast cancer molecular subtyping and treatment progress. Breast Cancer Res. 2020;22(1):61. doi:10.1186/s13058-020-01296-5
10. Fachal L, Aschard H, Beesley J, et al. Fine-mapping of 150 breast cancer risk regions identifies 191 likely target genes. Nat Genet. 2020;52(1):56–73. doi:10.1038/s41588-019-0537-1
11. Dorling L, Carvalho S, Allen J, et al.; Breast Cancer Association Consortium. Breast cancer risk genes-association analysis in more than 113,000 women. N Engl J Med. 2021;384(5):428–439.
12. Silvestris E, D’Oronzo S, Passarelli A, et al. Molecular assessment of ovarian cancer and translation to clinical management. In: Oncogenomics. Elsevier; 2019:501–519.
13. Chandra A, Pius C, Nabeel M, et al. Ovarian cancer: current status and strategies for improving therapeutic outcomes. Cancer Med. 2019;8(16):7018–7031. doi:10.1002/cam4.2560
14. Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H. Ovarian cancer in the world: epidemiology and risk factors. Int J Womens Health. 2019;11:287–299. doi:10.2147/IJWH.S197604
15. Hurwitz LM, Pinsky PF, Trabert B. General population screening for ovarian cancer. Lancet. 2021;397(10290):2128–2130. doi:10.1016/S0140-6736(21)01061-8
16. Delie F, Allemann E, Cohen M. Nanocarriers for ovarian cancer active drug targeting. J Drug Deliv Sci Technol. 2012;22(5):421–426. doi:10.1016/S1773-2247(12)50068-7
17. Kurnit KC, Fleming GF, Lengyel E. Updates and new options in advanced epithelial ovarian cancer treatment. Obstet Gynecol. 2021;137(1):108–121. doi:10.1097/AOG.0000000000004173
18. Golchin J, Golchin K, Alidadian N, et al. Nanozyme applications in biology and medicine: an overview. Artif Cells Nanomed Biotechnol. 2017;45(6):1–8. doi:10.1080/21691401.2017.1313268
19. Oronsky B, Ray CM, Spira AI, Trepel JB, Carter CA, Cottrill HM. A brief review of the management of platinum-resistant–platinum-refractory ovarian cancer. Med Oncol. 2017;34(6):103. doi:10.1007/s12032-017-0960-z
20. Bankhead CR, Collins C, Stokes-Lampard H, et al. Identifying symptoms of ovarian cancer: a qualitative and quantitative study. BJOG. 2008;115(8):1008–1014. doi:10.1111/j.1471-0528.2008.01772.x
21. Wellenstein MD, Coffelt SB, Duits DEM, et al. Loss of p53 triggers WNT-dependent systemic inflammation to drive breast cancer metastasis. Nature. 2019;572(7770):538–542. doi:10.1038/s41586-019-1450-6
22. Wei H, Wang E. Nanomaterials with enzyme-like characteristics (nanozymes): next-generation artificial enzymes. Chem Soc Rev. 2013;42(14):6060–6093. doi:10.1039/c3cs35486e
23. Gomaa EZ. Nanozymes: a promising horizon for medical and environmental applications. J Clust Sci. 2022;33(4):1275–1297. doi:10.1007/s10876-021-02079-4
24. Wu J, Wang X, Wang Q, et al. Nanomaterials with enzyme-like characteristics (nanozymes): next-generation artificial enzymes (II). Chem Soc Rev. 2019;48(4):1004–1076. doi:10.1039/c8cs00457a
25. Xia F, Shi Q, Nan Z. Facile synthesis of Cu-CuFe2O4 nanozymes for sensitive assay of H2O2 and GSH. Dalton Trans. 2020;49(36):12780–12792. doi:10.1039/D0DT02395G
26. Zhang Y, Jin Y, Cui H, Yan X, Fan K. Nanozyme-based catalytic theranostics. RSC Adv. 2019;10(1):10–20. doi:10.1039/C9RA09021E
27. Mandal A, Dasgupta S, Adhikary A, Samanta D, Zangrando E, Das D. Synthesis of Mn3O4 nanozymes from structurally characterized phenoxazinone synthase models based on manganese. Dalton Trans. 2020;49(18):5999–6011. doi:10.1039/D0DT00355G
28. Chong Y, Liu Q, Ge C. Advances in oxidase-mimicking nanozymes: classification, activity regulation and biomedical applications. Nano Today. 2021;37:101076. doi:10.1016/j.nantod.2021.101076
29. Wu Y, Wen J, Xu W, et al. Defect‐engineered nanozyme‐linked receptors. Small. 2021;17(33):2101907. doi:10.1002/smll.202101907
30. Wu Y, Darland DC, Zhao JX. Nanozymes—hitting the biosensing “target”. Sensors. 2021;21(15):5201. doi:10.3390/s21155201
31. Das B, Franco JL, Logan N, Balasubramanian P, Kim MI, Cao C. Nanozymes in point-of-care diagnosis: an emerging futuristic approach for biosensing. Nano Micro Lett. 2021;13(1):193.
32. Chan GG, Koch CM, Connors LH. Blood proteomic profiling in inherited (ATTRm) and acquired (ATTRwt) forms of transthyretin-associated cardiac amyloidosis. J Proteome Res. 2017;16(4):1659–1668. doi:10.1021/acs.jproteome.6b00998
33. Lu C, Liu X, Li Y, et al. Multifunctional Janus hematite-silica nanoparticles: mimicking peroxidase-like activity and sensitive colorimetric detection of glucose. ACS Appl Mater Interfaces. 2015;7(28):15395–15402. doi:10.1021/acsami.5b03423
34. Zhao Y, Ran W, He J, et al. High‐performance asymmetric supercapacitors based on multilayer MnO2/graphene oxide nanoflakes and hierarchical porous carbon with enhanced cycling stability. Small. 2015;11(11):1310–1319. doi:10.1002/smll.201401922
35. Jiang D, Ni D, Rosenkrans ZT, Huang P, Yan X, Cai W. Nanozyme: new horizons for responsive biomedical applications. Chem Soc Rev. 2019;48(14):3683–3704. doi:10.1039/c8cs00718g
36. Cao C, Zhang T, Yang N, et al. POD Nanozyme optimized by charge separation engineering for light/ pH activated bacteria catalytic/ photodynamic therapy. Signal Transduct Target Ther. 2022;7(1):1. doi:10.1038/s41392-021-00710-4
37. Yang H, Xu B, Li S, et al. A photoresponsive nanozyme for synergistic catalytic therapy and dual phototherapy. Small. 2021;17(10):e2007090. doi:10.1002/smll.202007090
38. Dai Z, Guo J, Xu J, Liu C, Gao Z, Song YY. Target-driven nanozyme growth in TiO2 nanochannels for improving selectivity in electrochemical biosensing. Anal Chem. 2020;92(14):10033–10041. doi:10.1021/acs.analchem.0c01815
39. Zhang R, Yan X, Fan K. Nanozymes inspired by natural enzymes. Acc Mater Res. 2021;2(7):534–547. doi:10.1021/accountsmr.1c00074
40. Song Y, Wang X, Zhao C, Qu K, Ren J, Qu X. Label-free colorimetric detection of single nucleotide polymorphism by using single-walled carbon nanotube intrinsic peroxidase-like activity. Chemistry. 2010;16(12):3617–3621. doi:10.1002/chem.200902643
41. Zhong Q, Chen Y, Su A, Wang Y. Synthesis of catalytically active carbon quantum dots and its application for colorimetric detection of glutathione. Sens Actuators B. 2018;273:1098–1102. doi:10.1016/j.snb.2018.07.026
42. Song J, Pandian V, Mauk MG, et al. Smartphone-based mobile detection platform for molecular diagnostics and spatiotemporal disease mapping. Anal Chem. 2018;90(7):4823–4831. doi:10.1021/acs.analchem.8b00283
43. Zeng L, Han Y, Chen Z, Jiang K, Golberg D, Weng Q. Biodegradable and peroxidase‐mimetic boron oxynitride nanozyme for breast cancer therapy. Adv Sci. 2021;8(16):e2101184. doi:10.1002/advs.202101184
44. Liu C, Cai Y, Wang J, et al. Facile preparation of homogeneous copper nanoclusters exhibiting excellent tetraenzyme mimetic activities for colorimetric glutathione sensing and fluorimetric ascorbic acid sensing. ACS Appl Mater Interfaces. 2020;12(38):42521–42530. doi:10.1021/acsami.0c11983
45. Hafez ME, Ma H, Ma W, Long YT. Unveiling the intrinsic catalytic activities of single‐gold‐nanoparticle‐based enzyme mimetics. Angew Chem. 2019;131(19):6393–6398. doi:10.1002/ange.201901384
46. Luo W, Zhu C, Su S, et al. Manuscript received. ACS Nano. 2017;31:7451–7458.
47. Cui M, Zhao Y, Wang C, Song Q. The oxidase-like activity of iridium nanoparticles, and their application to colorimetric determination of dissolved oxygen. Microchim Acta. 2017;184(9):3113–3119. doi:10.1007/s00604-017-2326-9
48. Wang D, Wu H, Wang C, et al. Self‐assembled single‐site nanozyme for tumor‐specific amplified cascade enzymatic therapy. Angew Chem. 2021;133(6):3038–3044. doi:10.1002/ange.202008868
49. Wang L, Zhang S, Wang X. The metabolic mechanisms of breast cancer metastasis. Front Oncol. 2020;10:602416. doi:10.3389/fonc.2020.602416
50. Asati A, Santra S, Kaittanis C, Nath S, Perez JM. Oxidase‐like activity of polymer‐coated cerium oxide nanoparticles. Angew Chem. 2009;121(13):2344–2348. doi:10.1002/ange.200805279
51. Han J, Liu K, Chang R, Zhao L, Yan X. Photooxidase‐mimicking nanovesicles with superior photocatalytic activity and stability based on amphiphilic amino acid and phthalocyanine co‐assembly. Angew Chem. 2019;131(7):2022–2026. doi:10.1002/ange.201811478
52. Zhao Y, Wang J, Cai X, Ding P, Lv H, Pei R. Metal-organic frameworks with enhanced photodynamic therapy: synthesis, erythrocyte membrane camouflage, and aptamer-targeted aggregation. ACS Appl Mater Interfaces. 2020;12(21):23697–23706. doi:10.1021/acsami.0c04363
53. Dan Q, Hu D, Ge Y, et al. Ultrasmall theranostic nanozymes to modulate tumor hypoxia for augmenting photodynamic therapy and radiotherapy. Biomater Sci. 2020;8(3):973–987. doi:10.1039/C9BM01742A
54. Comotti M, Della Pina C, Matarrese R, Rossi M. The catalytic activity of “naked” gold particles. Angew Chem Int Ed Engl. 2004;43(43):5812–5815. doi:10.1002/anie.200460446
55. Aoudj S, Khelifa A, Drouiche N, Belkada R, Miroud D. Simultaneous removal of chromium(VI) and fluoride by electrocoagulation–electroflotation: application of a hybrid Fe-Al anode. Chem Eng J. 2015;267:153–162. doi:10.1016/j.cej.2014.12.081
56. Liu CP, Wu TH, Liu CY, et al. Self‐supplying O2 through the catalase‐like activity of gold nanoclusters for photodynamic therapy against hypoxic cancer cells. Small. 2017;13(26):1700278. doi:10.1002/smll.201700278
57. Liu Y, Ding D, Zhen Y, Guo R. Amino acid-mediated’turn-off/turn-on’nanozyme activity of gold nanoclusters for sensitive and selective detection of copper ions and histidine. Biosens Bioelectron. 2017;92:140–146. doi:10.1016/j.bios.2017.01.036
58. Guo W, Zhang M, Lou Z, Zhou M, Wang P, Wei H. Engineering nanoceria for enhanced peroxidase mimics: a solid solution strategy. ChemCatChem. 2019;11(2):737–743. doi:10.1002/cctc.201801578
59. Huang Y, Liu Z, Liu C, et al. Self‐assembly of multi‐nanozymes to mimic an intracellular antioxidant defense system. Angew Chem. 2016;128(23):6758–6762. doi:10.1002/ange.201600868
60. Mu J, Zhao X, Li J, Yang EC, Zhao XJ. Novel hierarchical NiO nanoflowers exhibiting intrinsic superoxide dismutase-like activity. J Mater Chem B. 2016;4(31):5217–5221. doi:10.1039/c6tb01390b
61. Korsvik C, Patil S, Seal S, Self W. Vacancy engineered ceria oxide nanoparticles catalyze superoxide dismutase activity. Chem Commun. 2007;10:1056–1058. doi:10.1039/b615134e
62. Korsvik C, Patil S, Seal S, Self WT. Superoxide dismutase mimetic properties exhibited by vacancy engineered ceria nanoparticles. Chem Commun. 2007;10(10):1056–1058.
63. Zhang S, Zhang R, Yan X, Fan K. Nanozyme‐based artificial organelles: an emerging direction for artificial organelles. Small. 2022;18(33):e2202294.
64. Singh N, Geethika M, Eswarappa SM, Mugesh G. Manganese‐based nanozymes: multienzyme redox activity and effect on the nitric oxide produced by endothelial nitric oxide synthase. Chemistry. 2018;24(33):8393–8403. doi:10.1002/chem.201800770
65. Tian R, Sun J, Qi Y, Zhang B, Guo S, Zhao M. Influence of VO2 nanoparticle morphology on the colorimetric assay of H2O2 and glucose. Nanomaterials. 2017;7(11):347. doi:10.3390/nano7110347
66. Sun Z, Zhang N, Si Y, et al. High-throughput colorimetric assays for mercury (II). Chem Commun. 2014;50(65):9196–9199. doi:10.1039/C4CC03851G
67. Wu GW, He SB, Peng HP, et al. Citrate-capped platinum nanoparticle as a smart probe for ultrasensitive mercury sensing. Anal Chem. 2014;86(21):10955–10960. doi:10.1021/ac503544w
68. Fan Y, Shi W, Zhang X, Huang Y. Mesoporous material-based manipulation of the enzyme-like activity of CoFe2O4 nanoparticles. J Mater Chem A. 2014;2(8):2482–2486. doi:10.1039/c3ta14697a
69. Wang H, Liu C, Liu Z, Ren J, Qu X. Specific oxygenated groups enriched graphene quantum dots as highly efficient enzyme mimics. Small. 2018;14(13):e1703710.
70. Xu C, Bing W, Wang F, Ren J, Qu X. Versatile dual photoresponsive system for precise control of chemical reactions. ACS Nano. 2017;11(8):7770–7780. doi:10.1021/acsnano.7b01450
71. Moglianetti M, De Luca E, Pedone D, et al. Platinum nanozymes recover cellular ROS homeostasis in an oxidative stress-mediated disease model. Nanoscale. 2016;8(6):3739–3752. doi:10.1039/C5NR08358C
72. Ali SS, Hardt JI, Quick KL, et al. A biologically effective fullerene (C60) derivative with superoxide dismutase mimetic properties. Free Radic Biol Med. 2004;37(8):1191–1202. doi:10.1016/j.freeradbiomed.2004.07.002
73. Li F, Li N, Xue C, et al. A Cu2O-CDs-Cu three component catalyst for boosting oxidase-like activity with hot electrons. Chem Eng J. 2020;382:122484. doi:10.1016/j.cej.2019.122484
74. Hou J, Jia P, Yang K, Bu T, Sun X, Wang L. Facile preparation of Ru@V2O4 nanowires exhibiting excellent tetra-enzyme mimetic activities for sensitive colorimetric H2O2 and cysteine sensing. Sens Actuators B. 2021;344:130266. doi:10.1016/j.snb.2021.130266
75. Li Q, Wu T, Fan X, Guo X, Jiang W, Fan K. Multifaceted nanozymes for synergistic antitumor therapy: a review. Mater Des. 2022;224:111430. doi:10.1016/j.matdes.2022.111430
76. Li W, Zhang Q, Cai Y, Chen T, Cheng H. The COMT genetic factor regulates chemotherapy-related prospective memory impairment in survivors with HER2−/+ breast cancer. Front Oncol. 2022;12:816923. doi:10.3389/fonc.2022.816923
77. Kanwal Q, Shahid S, Ahmad A, et al. Sustainable, economical and rapid treatment of multiple lung diseases using therapeutic potential of curcumin nanoparticles. Environ Res. 2023;233:116477. doi:10.1016/j.envres.2023.116477
78. Muthukrishnan L. Disruptive nanozyme technology for futuristic bio-medical and bio-imaging applications. Curr Nanosci. 2021;17(6):853–870. doi:10.2174/1573413717666210216120328
79. Zhang W, Ma D, Du J. Prussian Blue nanoparticles as peroxidase mimetics for sensitive colorimetric detection of hydrogen peroxide and glucose. Talanta. 2014;120:362–367. doi:10.1016/j.talanta.2013.12.028
80. Liu H, Gu C, Xiong W, Zhang M. A sensitive hydrogen peroxide biosensor using ultra-small CuInS2 nanocrystals as peroxidase mimics. Sens Actuators B. 2015;209:670–676. doi:10.1016/j.snb.2014.12.052
81. Zhang X, He S, Chen Z, Huang Y. CoFe2O4 nanoparticles as oxidase mimic-mediated chemiluminescence of aqueous luminol for sulfite in white wines. J Agric Food Chem. 2013;61(4):840–847. doi:10.1021/jf3041269
82. Baldim V, Bedioui F, Mignet N, Margaill I, Berret JF. The enzyme-like catalytic activity of cerium oxide nanoparticles and its dependency on Ce3+ surface area concentration. Nanoscale. 2018;10(15):6971–6980. doi:10.1039/C8NR00325D
83. Wang L, Zhou H, Hu H, Wang Q, Chen X. Regulation mechanism of ssDNA aptamer in nanozymes and application of nanozyme-based aptasensors in food safety. Foods. 2022;11(4):544. doi:10.3390/foods11040544
84. Zhang W, Dong J, Wu Y, et al. Shape-dependent enzyme-like activity of Co3O4 nanoparticles and their conjugation with his-tagged EGFR single-domain antibody. Colloids Surf B Biointerfaces. 2017;154:55–62. doi:10.1016/j.colsurfb.2017.02.034
85. Peng FF, Zhang Y, Gu N. Size-dependent peroxidase-like catalytic activity of Fe3O4 nanoparticles. Chin Chem Lett. 2008;19(6):730–733. doi:10.1016/j.cclet.2008.03.021
86. Wu J, Qin K, Yuan D, et al. Rational design of Au@Pt multibranched nanostructures as bifunctional nanozymes. ACS Appl Mater Interfaces. 2018;10(15):12954–12959. doi:10.1021/acsami.7b17945
87. Zhu A, Sun K, Petty HR. Titanium doping reduces superoxide dismutase activity, but not oxidase activity, of catalytic CeO2 nanoparticles. Inorg Chem Commun. 2012;15:235–237. doi:10.1016/j.inoche.2011.10.034
88. Zhang X-Q, Gong S-W, Zhang Y, Yang T, Wang C-Y, Gu N. Prussian Blue modified iron oxide magnetic nanoparticles and their high peroxidase-like activity. J Mater Chem. 2010;20(24):5110–5116. doi:10.1039/c0jm00174k
89. Zhang W, Hu S, Yin JJ, et al. Prussian Blue nanoparticles as multienzyme mimetics and reactive oxygen species scavengers. J Am Chem Soc. 2016;138(18):5860–5865. doi:10.1021/jacs.5b12070
90. Tan B, Zhang S, Wang K, et al. Moisture-resistant and green cyclodextrin metal-organic framework nanozyme based on cross-linkage for visible detection of cellular hydrogen peroxide. Mikrochim Acta. 2022;189(8):295. doi:10.1007/s00604-022-05389-0
91. Meng X, Fan K, Yan X. Nanozymes: an emerging field bridging nanotechnology and enzymology. Sci China Life Sci. 2019;62(11):1543–1546. doi:10.1007/s11427-019-1557-8
92. Ou D, Sun D, Lin X, Liang Z, Zhong Y, Chen Z. A dual-aptamer-based biosensor for specific detection of breast cancer biomarker HER2 via flower-like nanozymes and DNA nanostructures. J Mater Chem B. 2019;7(23):3661–3669. doi:10.1039/C9TB00472F
93. Wei C, Liu Y, Zhu X, et al. Iridium/ruthenium nanozyme reactors with cascade catalytic ability for synergistic oxidation therapy and starvation therapy in the treatment of breast cancer. Biomaterials. 2020;238:119848. doi:10.1016/j.biomaterials.2020.119848
94. Wang YM, Liu JW, Adkins GB, et al. Enhancement of the intrinsic peroxidase-like activity of graphitic carbon nitride nanosheets by ssDNAs and its application for detection of exosomes. Anal Chem. 2017;89(22):12327–12333. doi:10.1021/acs.analchem.7b03335
95. Fan K, Cao C, Pan Y, et al. Magnetoferritin nanoparticles for targeting and visualizing tumour tissues. Nat Nanotechnol. 2012;7(7):459–464. doi:10.1038/nnano.2012.90
96. Yang X, Stein EW, Ashkenazi S, Wang LV. Nanoparticles for photoacoustic imaging. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2009;1(4):360–368. doi:10.1002/wnan.42
97. Ding H, Cai Y, Gao L, et al. Exosome-like nanozyme vesicles for H2O2-responsive catalytic photoacoustic imaging of xenograft nasopharyngeal carcinoma. Nano Lett. 2018;19(1):203–209. doi:10.1021/acs.nanolett.8b03709
98. Loynachan CN, Soleimany AP, Dudani JS, et al. Renal clearable catalytic gold nanoclusters for in vivo disease monitoring. Nat Nanotechnol. 2019;14(9):883–890. doi:10.1038/s41565-019-0527-6
99. Xi J, Xie C, Zhang Y, et al. Pd nanoparticles decorated N-doped graphene quantum dots@N-doped carbon hollow nanospheres with high electrochemical sensing performance in cancer detection. ACS Appl Mater Interfaces. 2016;8(34):22563–22573. doi:10.1021/acsami.6b05561
100. Ye Y, Xiao L, He B, et al. Oxygen-tuned nanozyme polymerization for the preparation of hydrogels with printable and antibacterial properties. J Mater Chem B. 2017;5(7):1518–1524. doi:10.1039/C6TB03317B
101. Li N, Deng Y, Zhou L, et al. Global burden of breast cancer and attributable risk factors in 195 countries and territories, from 1990 to 2017: results from the Global Burden of Disease Study 2017. J Hematol Oncol. 2019;12(1):1–12. doi:10.1186/s13045-019-0828-0
102. Li S, Shang L, Xu B, et al. A nanozyme with photo‐enhanced dual enzyme‐like activities for deep pancreatic cancer therapy. Angew Chem. 2019;131(36):12754–12761. doi:10.1002/ange.201904751
103. Ding S-S, He L, Bian X-W, Tian G. Metal-organic frameworks-based nanozymes for combined cancer therapy. Nano Today. 2020;35:100920. doi:10.1016/j.nantod.2020.100920
104. Fan K, Xi J, Fan L, et al. In vivo guiding nitrogen-doped carbon nanozyme for tumor catalytic therapy. Nat Commun. 2018;9(1):1–11. doi:10.1038/s41467-018-03903-8
105. An Q, Sun C, Li D, Xu K, Guo J, Wang C. Peroxidase-like activity of Fe3O4@carbon nanoparticles enhances ascorbic acid-induced oxidative stress and selective damage to PC-3 prostate cancer cells. ACS Appl Mater Interfaces. 2013;5(24):13248–13257. doi:10.1021/am4042367
106. Huang G, Chen H, Dong Y, et al. Superparamagnetic iron oxide nanoparticles: amplifying ROS stress to improve anticancer drug efficacy. Theranostics. 2013;3(2):116–126. doi:10.7150/thno.5411
107. Jiang Z, Chen X, Lin Y, et al. Synergistic approach to combat triple‐negative breast cancer: B7‐H4 checkpoint‐based photodynamic nanodrug coupled with neutrophil extracellular trap regulation. Adv Funct Mater. 2023;33(51):2307756. doi:10.1002/adfm.202307756
108. Vakili-Ghartavol R, Momtazi-Borojeni AA, Vakili-Ghartavol Z, et al. Toxicity assessment of superparamagnetic iron oxide nanoparticles in different tissues. Artif Cells Nanomed Biotechnol. 2020;48(1):443–451. doi:10.1080/21691401.2019.1709855
109. Huo M, Wang L, Chen Y, Shi J. Tumor-selective catalytic nanomedicine by nanocatalyst delivery. Nat Commun. 2017;8(1):357. doi:10.1038/s41467-017-00424-8
110. Yang L, Ren C, Xu M, et al. Rod-shape inorganic biomimetic mutual-reinforcing MnO2-Au nanozymes for catalysis-enhanced hypoxic tumor therapy. Nano Res. 2020;13(8):2246–2258. doi:10.1007/s12274-020-2844-3
111. Sun L, Gao W, Liu J, et al. O2-supplying nanozymes alleviate hypoxia and deplete lactate to eliminate tumors and activate antitumor immunity. ACS Appl Mater Interfaces. 2022;14(51):56644–56657. doi:10.1021/acsami.2c18960
112. Zheng H, Wang S, Zhou L, et al. Injectable multi-responsive micelle/nanocomposite hybrid hydrogel for bioenzyme and photothermal augmented chemodynamic therapy of skin cancer and bacterial infection. Chem Eng J. 2021;404:126439. doi:10.1016/j.cej.2020.126439
113. Dos Santos AF, de Almeida DQ, Terra LF, Baptista MS, Labriola L. Photodynamic therapy in cancer treatment-an update review. J Cancer Metast Treat. 2019;5:25.
114. Zhu W, Dong Z, Fu T, et al. Modulation of hypoxia in solid tumor microenvironment with MnO2 nanoparticles to enhance photodynamic therapy. Adv Funct Mater. 2016;26(30):5490–5498. doi:10.1002/adfm.201600676
115. Giacco F, Brownlee M, Schmidt AM. Oxidative stress and diabetic complications. Circ Res. 2010;107(9):1058–1070. doi:10.1161/CIRCRESAHA.110.223545
116. Grulke E, Reed K, Beck M, Huang X, Cormack A, Seal S. Nanoceria: factors Affecting Its pro- and anti-Oxidant Properties. Environ Sci Nano. 2014;1(5):429–444. doi:10.1039/C4EN00105B
117. Safi H, Lingaraju S, Ma S, et al. Rapidly correcting frameshift mutations in the Mycobacterium tuberculosis Orn Gene produce reversible ethambutol resistance and small-colony-variant morphology. Antimicrob Agents Chemother. 2020;64(9):e00213–20. doi:10.1128/AAC.00213-20
118. Alili L, Sack M, Karakoti AS, et al. Combined cytotoxic and anti-invasive properties of redox-active nanoparticles in tumor–stroma interactions. Biomaterials. 2011;32(11):2918–2929. doi:10.1016/j.biomaterials.2010.12.056
119. Wang M, Guo X, Yang X, et al. Mycobacterial dynamin-like protein IniA mediates membrane fission. Nat Commun. 2019;10(1):3906. doi:10.1038/s41467-019-11860-z
120. Das J, Choi YJ, Han JW, Reza AMMT, Kim JH. Nanoceria-mediated delivery of doxorubicin enhances the anti-tumour efficiency in ovarian cancer cells via apoptosis. Sci Rep. 2017;7(1):9513. doi:10.1038/s41598-017-09876-w
121. Giri S, Karakoti A, Graham RP, et al. Nanoceria: a rare-earth nanoparticle as a novel anti-angiogenic therapeutic agent in ovarian cancer. PLoS One. 2013;8(1):e54578. doi:10.1371/journal.pone.0054578
122. Vassie JA, Whitelock JM, Lord MS. Endocytosis of cerium oxide nanoparticles and modulation of reactive oxygen species in human ovarian and colon cancer cells. Acta Biomater. 2017;50:127–141. doi:10.1016/j.actbio.2016.12.010
123. Yan X, ed.. Nanozymology: Connecting Biology and Nanotechnology. Springer Singapore; 2020.
124. Conklin KA. Chemotherapy-associated oxidative stress: impact on chemotherapeutic effectiveness. Integr Cancer Ther. 2004;3(4):294–300. doi:10.1177/1534735404270335
125. Noguera-Troise I, Daly C, Papadopoulos NJ, et al. Blockade of Dll4 inhibits tumour growth by promoting non-productive angiogenesis. Nature. 2006;444(7122):1032–1037. doi:10.1038/nature05355
126. Wang Z, Dabrosin C, Yin X, et al. Broad targeting of angiogenesis for cancer prevention and therapy. Semin Cancer Biol. 2015;35(suppl):S224–S243. doi:10.1016/j.semcancer.2015.01.001
127. Hijaz M, Das S, Mert I, et al. Folic acid tagged nanoceria as a novel therapeutic agent in ovarian cancer. BMC Cancer. 2016;16(1):220. doi:10.1186/s12885-016-2206-4
128. He X, Zhang H, Ma Y, et al. Lung deposition and extrapulmonary translocation of nano-ceria after intratracheal instillation. Nanotechnology. 2010;21(28):285103. doi:10.1088/0957-4484/21/28/285103
129. Iyer AK, Singh A, Ganta S, Amiji MM. Role of integrated cancer nanomedicine in overcoming drug resistance. Adv Drug Deliv Rev. 2013;65(13–14):1784–1802. doi:10.1016/j.addr.2013.07.012
130. Guo C, Zou J, Wen Y, et al. Apical cell-cell adhesions reconcile symmetry and asymmetry in zebrafish neurulation. iScience. 2018;3:63–85. doi:10.1016/j.isci.2018.04.007
131. Risnayanti C, Jang Y-S, Lee J, Ahn HJ. PLGA nanoparticles co-delivering MDR1 and BCL2 SiRNA for overcoming resistance of paclitaxel and cisplatin in recurrent or advanced ovarian cancer. Sci Rep. 2018;8(1):7498. doi:10.1038/s41598-018-25930-7
132. Winterbourn CC. Toxicity of iron and hydrogen peroxide: the Fenton reaction. Toxicol Lett. 1995;82–83:969–974. doi:10.1016/0378-4274(95)03532-X
133. Korschelt K, Tahir MN, Tremel W. A step into the future: applications of nanoparticle enzyme mimics. Chemistry. 2018;24(39):9703–9713. doi:10.1002/chem.201800384
134. Alphandéry E. Iron oxide nanoparticles for therapeutic applications. Drug Discov Today. 2020;25(1):141–149. doi:10.1016/j.drudis.2019.09.020
135. Zhang D, Zhao YX, Gao YJ, et al. Anti-bacterial and in vivo tumor treatment by reactive oxygen species generated by magnetic nanoparticles. J Mater Chem B. 2013;1(38):5100–5107. doi:10.1039/c3tb20907e
136. Saikia C, Das MK, Ramteke A, Maji TK. Effect of crosslinker on drug delivery properties of curcumin loaded starch coated iron oxide nanoparticles. Int J Biol Macromol. 2016;93(A):1121–1132. doi:10.1016/j.ijbiomac.2016.09.043
137. Liang S, Deng X, Ma P, Cheng Z, Lin J. Recent advances in nanomaterial‐assisted combinational sonodynamic cancer therapy. Adv Mater. 2020;32(47):e2003214. doi:10.1002/adma.202003214
138. Gao L, Zhuang J, Nie L, et al. Intrinsic peroxidase-like activity of ferromagnetic nanoparticles. Nat Nanotechnol. 2007;2(9):577–583. doi:10.1038/nnano.2007.260
139. Dhani N, Fyles A, Hedley D, Milosevic M. The clinical significance of hypoxia in human cancers. Semin Nucl Med. 2015;45(2):110–121. doi:10.1053/j.semnuclmed.2014.11.002
140. Wang X, Hu Y, Wei H. Nanozymes in bionanotechnology: from sensing to therapeutics and beyond. Inorg Chem Front. 2016;3(1):41–60. doi:10.1039/C5QI00240K
141. Sahu A, Kwon I, Tae G. Improving cancer therapy through the nanomaterials-assisted alleviation of hypoxia. Biomaterials. 2020;228:119578. doi:10.1016/j.biomaterials.2019.119578
142. Tan S, Wu T, Zhang D, Zhang Z. Cell or cell membrane-based drug delivery systems. Theranostics. 2015;5(8):863–881. doi:10.7150/thno.11852
143. Ma A, Chen H, Cui Y, et al. Metalloporphyrin complex‐based nanosonosensitizers for deep‐tissue tumor theranostics by noninvasive sonodynamic therapy. Small. 2019;15(5):e1804028. doi:10.1002/smll.201804028
144. Hada A-M, Craciun A-M, Focsan M, et al. Folic acid functionalized gold nanoclusters for enabling targeted fluorescence imaging of human ovarian cancer cells. Talanta. 2021;225:121960. doi:10.1016/j.talanta.2020.121960
145. Liang Y, Zhang H, Song X, Yang Q. Metastatic heterogeneity of breast cancer: molecular mechanism and potential therapeutic targets. Semin Cancer Biol. 2020;60:14–27. doi:10.1016/j.semcancer.2019.08.012
146. Cha S-H, Hong J, McGuffie M, Yeom B, VanEpps JS, Kotov NA. Shape-dependent biomimetic inhibition of enzyme by nanoparticles and their antibacterial activity. ACS Nano. 2015;9(9):9097–9105. doi:10.1021/acsnano.5b03247
147. Tripathi RM, Ahn D, Kim YM, Chung SJ. Enzyme mimetic activity of ZnO-Pd nanosheets synthesized via a green route. Molecules. 2020;25(11):2585. doi:10.3390/molecules25112585
148. Sobańska K, Pietrzyk P, Sojka Z. Generation of reactive oxygen species via electroprotic interaction of H2O2 with ZrO2 gel: ionic sponge effect and pH-switchable peroxidase- and catalase-like activity. ACS Catal. 2017;7(4):2935–2947. doi:10.1021/acscatal.7b00189
149. Miao W, Kim H, Gujrati V, et al. Photo-decomposable organic nanoparticles for combined tumor optical imaging and multiple phototherapies. Theranostics. 2016;6(13):2367–2379. doi:10.7150/thno.15829
150. Choi W, Park EY, Jeon S, Kim C. Clinical photoacoustic imaging platforms. Biomed Eng Lett. 2018;8(2):139–155. doi:10.1007/s13534-018-0062-7
151. Siddique S, Chow JCL. Application of nanomaterials in biomedical imaging and cancer therapy. Nanomaterials. 2020;10(9):1700. doi:10.3390/nano10091700
152. Arshad F, Mohd-Naim NF, Chandrawati R, Cozzolino D, Ahmed MU. Nanozyme-based sensors for detection of food biomarkers: a review. RSC Adv. 2022;12(40):26160–26175. doi:10.1039/D2RA04444G
153. Prasad P, Gordijo CR, Abbasi AZ, et al. Multifunctional albumin-MnO2 nanoparticles modulate solid tumor microenvironment by attenuating hypoxia, acidosis, vascular endothelial growth factor and enhance radiation response. ACS Nano. 2014;8(4):3202–3212. doi:10.1021/nn405773r
154. Ma P, Xiao H, Yu C, et al. Enhanced cisplatin chemotherapy by iron oxide nanocarrier-mediated generation of highly toxic reactive oxygen species. Nano Lett. 2017;17(2):928–937. doi:10.1021/acs.nanolett.6b04269
155. Meng X, Li D, Chen L, et al. High-performance self-cascade pyrite nanozymes for apoptosis–ferroptosis synergistic tumor therapy. ACS Nano. 2021;15(3):5735–5751. doi:10.1021/acsnano.1c01248
156. Iqbal MA, Malik M, Le TK, et al. Technological evolution of image sensing designed by nanostructured materials. ACS Mater Lett. 2023;5(4):1027–1060. doi:10.1021/acsmaterialslett.2c01011
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

