Back to Journals » Clinical Ophthalmology » Volume 18
Noninvasive Ocular Surface Workup in Patients with Meibomian Gland Dysfunction Using Microwave-Heated Eye Bag
Authors Rossi C, Vaccaro S, Borselli M, Carnovale Scalzo G, Toro MD , Scorcia V, Giannaccare G
Received 19 December 2023
Accepted for publication 20 February 2024
Published 18 March 2024 Volume 2024:18 Pages 853—858
DOI https://doi.org/10.2147/OPTH.S451925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Costanza Rossi,1,* Sabrina Vaccaro,1,* Massimiliano Borselli,1 Giovanna Carnovale Scalzo,1 Mario Damiano Toro,2 Vincenzo Scorcia,1 Giuseppe Giannaccare3
1Department of Ophthalmology, University Magna Graecia of Catanzaro, Catanzaro, Italy; 2Eye Clinic, Public Health Department, University of Naples Federico II, Naples, Italy; 3Eye Clinic, Department of Surgical Sciences, University of Cagliari, Cagliari, Italy
*These authors contributed equally to this work
Correspondence: Giuseppe Giannaccare, Ophthalmology, Chairman of Eye Clinic, Department of Surgical Sciences, University of Cagliari, Cagliari, Italy, Email [email protected]
Purpose: To report the outcomes of a novel microwave heating device (Blepha EyeBag®) used serially for the treatment of meibomian gland dysfunction (MGD).
Patients and Methods: This prospective single center study was conducted at University Magna Graecia of Catanzaro. Patients were instructed to apply the compress twice daily for 15 days and once per day every two days, as reported in the package insert. Outcome measures were i) ocular surface disease index (OSDI) score, ii) tear meniscus height (TMH), iii) non-invasive keratograph break-up time (NIKBUT) (first and average), iv) meiboscore, v) bulbar redness. Evaluations were performed at baseline (T0) after 15 days (T1) and after 45 days of therapy (T2).
Results: Overall, 19 patients with MGD (8 males, 11 females; mean age 64.58 ± 9.72 years) were included. The mean value of OSDI score showed a significant decrease from 28.16 ± 17.46 at T0 to 13.69 ± 7.62 at T2 (p=0.008). The mean value of NIKBUT first significantly increased from 6.67 ± 3.51 seconds (s) at T0 to 10.46 ± 4.64 at T2 (p=0.0121); in parallel, the mean value of NIKBUT average increased significantly from 11.09 ± 4.15 s at T0 to 14.95 ± 4.85 at T2 (p=0.0049). No significant differences were detected at each time point for bulbar redness, meiboscore and TMH. Throughout the entire study, no adverse events were recorded.
Conclusion: The microwave-heated eye bag treatment is both safe and effective for treatment of MGD, being able to significantly ameliorate both patient-reported symptoms and tear film stability.
Keywords: MGD, dry eye, ocular surface disease, warming device, eyelid
Introduction
Blepharitis is a chronic inflammatory condition of the eyelid margins. Despite being frequently underdiagnosed, it affects a substantial portion of the global population and is reported in up to 47% of patients undergoing ophthalmological examinations.1,2 Reported symptoms include itching, redness, foreign body sensation, oftentimes exacerbating coexisting ocular surface diseases as allergic conjunctivitis and dry eye disease.3
Traditionally, blepharitis is classified into anterior and posterior forms. Anterior blepharitis is a condition of the eyelash bases and their follicles, while posterior blepharitis affects the inner rim of the eyelids, with meibomian gland dysfunction (MGD) often identified as the primary cause.2,3 Conventional therapy is addressed at controlling symptoms using warm compresses, eyelid hygiene, topical and/or oral antibiotics and anti-inflammatory agents (eg, corticosteroids) according to disease severity.4,5
Eyelid hygiene with warm compresses is paramount for clearing the orifices of the meibomian glands, allowing the spread of meibum in the tear film. Various warming devices have been designed to improve treatment comfort and compliance and have been shown to be successful for the treatment of MGD and chalazion.6–8
Herein, we report the outcomes of a novel microwave-heated flaxseed eye bag (Blepha EyeBag®, Theà Pharma, France) designed for at-home treatment of MGD and used continuously for 45 days according to the instructions reported in the package insert.
Materials and Methods
Study and Patients
This prospective study was conducted at University Magna Graecia of Catanzaro between June 2022 and August 2023. The study was approved by the local Ethics Committee (Comitato Etico Regione Calabria – Sezione Area Centro) and followed the tenets of the Declaration of Helsinki. Before performing any procedure, patients read, understood, and signed the informed consent. Patients over the age of 18 visiting the ocular surface clinic for regular check-ups were systematically assessed for eligibility. Inclusion criteria were diagnosis of MGD whose clinical signs and symptoms were not adequately managed despite first line therapy (unpreserved tear substitutes, eyelid hygiene with warm compresses); pathological values of Ocular Surface Disease Index (OSDI) score (≥13).
Exclusion criteria were systemic disease or therapies affecting tear secretion, other ocular diseases or use of topical drugs (eg, corticosteroids); recent (within 3 months) ocular surgery; history of contact lens wearing and eyelid malposition.
Patients were evaluated with a comprehensive examination at 3 time points: baseline (T0), 14 ± 2 days of treatment (T1) and 45 ± 4 days of treatment (T2). Noninvasive ocular surface examination was carried out by means of Oculus Keratograph 5 M (K5 M; Oculus GmbH, Wetzlar, Germany). This all-in-one device allowed for the measurement of i) tear meniscus height (TMH); ii) noninvasive Keratograph break-up time measured as the first distortion the 22 concentric rings reflected on the corneal surface (NIKBUT FIRST); iii) average time of all tear film break-ups occurring in the measured period of up to 24.98 seconds (s) (time limit set by the device’s software) (NIKBUT average); iv) infrared meibography; v) bulbar redness. Evaluation was carried out by a skilled examiner (S.V.). All measurements were conducted during a single visit in a dimly illuminated room, where the temperature was kept within the range of 21–24 °C and the humidity was maintained between 30–60%. Infrared meibography on lower eyelids was performed to assess meiboscore, a grading system which categorizes the extent of gland deficiency on a scale ranging from 0 to 3. Specifically, grade 0 indicated the absence of gland loss, grade 1 denoted gland loss that involves up to 33% of the total gland area, grade 2 represented gland loss ranging between 33% and 66%, and grade 3 indicated gland loss of 67% or more. Symptoms of ocular discomfort were assessed by means of Ocular Surface Disease Index (OSDI) questionnaire. The latter is a 12-item questionnaire assessing 3 aspects of symptomatology: vision-related function, ocular symptoms, and environmental triggers. Each response is given score from 0 to 4, with 0 indicating “none of the time” and 4 corresponding to “all of the time”. The sum of all values provides the OSDI score that ranges from 0 to 100. A score of 13 or more is considered pathological.
Study Treatment
Patients enrolled in the study were instructed to consistently use the eye bag throughout the study period. Given that the compress requires microwave heating, they were trained to heat it at the highest power setting for one minute. The optimal heating time for the device in a microwave oven varies depending on its power level. For microwaves with a power greater than 750 W, a 30-second heating period is advised. Conversely, for microwaves with a power of 750 W or less, a 40-second heating duration is recommended. To ensure even distribution of the flaxseeds within the eye bag and to facilitate effective heat dissipation, patients were advised to gently shake the device before use. Subsequently, the compress was to be applied over closed eyelids for the treatment.
According to the instructions contained in the package insert, the device was used twice daily for 5 to 10 minutes during the initial two-week period (T0 to T1); then, it was used every other day from T1 to T2.
All patients were instructed to maintain unchanged the ongoing therapy with unpreserved tear substitutes (1 drop three times daily).
Main Outcomes
The improvement in OSDI score following the treatment was the main outcome measure. An increase in NIKBUT first and average at T2 was considered as the secondary outcome measure.
Sample Size
In order to ascertain the necessary sample size for the investigation, a pre-existing power analysis was conducted utilizing the data from the study conducted by Piyacomn et al.9 Based on the above assumption, a sample size of 17 patients was determined to be necessary in order to detect a mean change of 14.5 points in the OSDI from its baseline level. The desired statistical power was set at 0.80, and the significance level (P value) was set at 0.05.
Statistical Analysis
Statistical analysis was performed using Prism version 9.5.0 (GraphPad Software Inc., San Diego, California, USA). Data were expressed as mean ± standard deviation (SD) if normally distributed, otherwise as median values with interquartile range (IQR). Anderson–Darling test and Kolmogorov–Smirnov tests were applied to assess if data were normally distributed. Student’s t-test or Mann–Whitney U-test was applied to compare variables when appropriate. A one-way ANOVA was calculated to determine whether the change of OSDI and NIKBUT first, NIKBUT average and TMH over time occurred. A p value of less than 0.05 was considered statistically significant.
Results
A total of 19 patients with anterior and/or posterior blepharitis (8 males, 11 females; mean age 64.58 ± 9.72 years) was included in the study. The mean value of OSDI score showed a significant decrease from 28.16 ± 17.46 at T0 to 16.05 ± 10.23 at T1 (p=0.0286) and 13.69 ± 7.62 at T2 (p=0.008) (Figure 1). The mean value of NIKBUT first significantly increased from 6.67 ± 3.51 s at T0 to 10.46 ± 4.64 at T2 (p=0.0121). Conversely, there were no statistically significant differences in NIKBUT first from T0 to T1 and from T1 to T2 (Table 1). In parallel, the mean value of NIKBUT average increased significantly from 11.09 ± 4.15 s at T0 to 14.74 ± 5.03 at T1 (p=0.0171) and 14.95 ± 4.85 at T2 (p=0.0049) (Figure 2). No differences (always p>0.5) were detected at each time point for bulbar redness, MGD and TMH (Table 1). Throughout the whole study, no adverse events were documented.
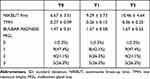 |
Table 1 Mean ± SD for NIKBUT First, TMH, BULBAR REDNESS and Meiboscore at T0, T1 and T2 |
 |
Figure 1 With respect to baseline (T0), OSDI score significantly decreased at both study time points, T1 and T2 (*p < 0.05, **p < 0.01). |
 |
Figure 2 With respect to baseline (T0), NIKBUT first significantly increased at T2 (*p < 0.05) while NIKBUT average increased at T1 (*p < 0.05) and at T2 (**p < 0.01). |
Discussion
This study assessed the effectiveness of a microwave-heated eye bag, formerly known as MGDRx EyeBag, used according to the instructions outlined in the package insert. This innovative heating device is specifically tailored for home treatment of dry eye disease owing to MGD and is designed to be used twice daily for 15 days, then once every other day for one month. Significant improvements were noted in patient-reported symptoms, as subjectively evaluated through the OSDI questionnaire, and in tear film stability, objectively assessed by the NIKBUT first and average measurements. These improvements were evident from the initial follow-up, two weeks after treatment commenced, and maintained nearly normal levels throughout the study and until the last follow-up, when the difference reached statistical significance. Conversely, the other parameters, namely TMH, MGD and bulbar redness, did not vary significantly. Regarding treatment safety and tolerability, no adverse events or side effects were reported by treated patients during the entire study.
Warm compresses have become a standard approach for ocular surface disease, and MGD in particular. However, such measures require sustained adherence to therapy over an extended time-period to achieve satisfactory results, potentially jeopardizing patient fulfilling. In this study, first beneficial effects were noted as soon as 15 days from the start of treatment, indicating the potential inclusion of this device in the therapeutic armamentarium for eyelid treatment. Indeed, heat therapy has been demonstrated to enhance meibum availability in the tear film, ameliorating its stability and prolonging tear break-up time in patients affected by MGD.10,11 Furthermore, in cases with Demodex infestation, these species are also tackled with heat, as the parasite is not capable of proliferating with temperatures of 37°C or above and is unable to survive at 54°C.12 Finally, elevated temperatures soften eyelash debris with beneficial effects in patients affected by blepharitis other than Demodex.
The continuous development of different devices has led to the conduction of various studies aimed at evaluating their effectiveness. A study conducted by Bilkhu et al evaluated eyelid temperature change and short-term effects on tear film stability and lipid layer thickness in healthy patients, using the microwave-heated eye bag.13 Their results highlighted a significant increase of eyelid temperatures, noninvasive break-up time (NIBUT), and lipid layer thickness immediately after the removal of the eye bag as well as 10 minutes later. Murphy et al compared the same device with warm face cloths and a moistening heating bag.14 Both devices showed superior efficacy in treating blepharitis compared to warm face cloth in terms of ocular surface staining and in meibum quality; however, differently from our data, no significant variation in NIBUT was detected in their study. Olafsson et al compared another micro-wave heated device containing gel beads to steam-based technology for the treatment of MGD.15 Their results highlighted that breakup time increased significantly and OSDI score decreased in both groups, with no difference among treatments. Yet, steam-based devices are considerably more expensive and less comfortable than microwave-based technologies; thus, given their equal efficacy, it is worth considering the use of microwave-heated devices in clinical practice. García-Marqués at al. assessed the correlation between the use of the microwave-heated eye bag and the improvement of dry eye signs and symptoms in young and older subjects. Following a two-week period of daily self-application to both eyes, in repeated cycles, the administration of heat bags resulted in the amelioration of symptoms associated with dry eye. However, improvements in NIKBUT and lipid layer thickness were observed exclusively in the younger participants.16 In another study, heat was administered concurrently to one eye using a portable heated eye mask, while the contralateral eye received heat through the microwave-heated eye bag. The latter was the preferred modality of therapy among the study participants.17
To the best of our knowledge, this is the first study evaluating effects of a novel microwave-heated eye bag used according to the new protocol described in the package insert using noninvasive technologies. However, this study suffers from some limitations including the short duration of the therapeutic scheme and the lack of a control group. Moreover, subjects were applying therapy at home, which may imply inadequate administration, despite thorough explanation at the time of prescription.
Conclusion
This prospective study demonstrated that microwave-heated flaxseed eye bag treatment, applied twice daily for 15 days and subsequently once every two days for 30 days, is both safe and effective. It notably reduces patient-reported symptoms of blepharitis and enhances tear film stability in affected individuals. Further studies with greater sample size and longer follow-ups are warranted for better evaluating the effect of this novel device on chronic blepharitis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lemp MA, Nichols KK. Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocul Surf. 2009;7(2 Suppl):S1–S14. doi:10.1016/S1542-0124(12)70620-1
2. Amescua G, Akpek EK, Farid M, et al. American Academy of Ophthalmology preferred practice pattern cornea and external disease panel. Blepharitis preferred practice pattern®. Ophthalmology. 2019;126(1):P56–P93.
3. Ayres BD, Donnenfeld E, Farid M, et al. Clinical diagnosis and management of demodex blepharitis: the Demodex Expert Panel on Treatment and Eyelid Health (DEPTH). Eye. 2023;37(15):3249–3255. doi:10.1038/s41433-023-02500-4
4. Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014;12(4):273–284. doi:10.1016/j.jtos.2014.05.005
5. Lindsley K, Matsumura S, Hatef E, et al. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012;2012(5):CD005556. doi:10.1002/14651858.CD005556.pub2
6. Mori A, Shimazaki J, Shimmura S, et al. Disposable eyelid-warming device for the treatment of meibomian gland dysfunction. Jpn J Ophthalmol. 2003;47(6):578–586. doi:10.1016/S0021-5155(03)00142-4
7. Ishida R, Matsumoto Y, Onguchi T, et al. Tear film with ”Orgahexa EyeMasks” in patients with meibomian gland dysfunction. Optom Vis Sci. 2008;85(8):E684–91. doi:10.1097/OPX.0b013e318181ae83
8. Matsumoto Y, Dogru M, Goto E, et al. Efficacy of a new warm moist air device on tear functions of patients with simple meibomian gland dysfunction. Cornea. 2006;25(6):644–650. doi:10.1097/01.ico.0000208822.70732.25
9. Piyacomn Y, Kasetsuwan N, Reinprayoon U, et al. Efficacy and safety of intense pulsed light in patients with meibomian gland dysfunction—a randomized, double-masked, sham-controlled clinical trial. Cornea. 2020;39(3):325–332. doi:10.1097/ICO.0000000000002204
10. Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 2003;29(2):96–99. doi:10.1097/01.ICL.0000060998.20142.8D
11. Goto E, Monden Y, Takano Y, et al. Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br J Ophthalmol. 2002;86(12):1403–1407. doi:10.1136/bjo.86.12.1403
12. Murube J. Demodex hominis. Ocul Surf. 2015;13(3):181–186. doi:10.1016/j.jtos.2015.04.002
13. Bilkhu PS, Naroo SA, Wolffsohn JS. Effect of a commercially available warm compress on eyelid temperature and tear film in healthy eyes. Optom Vis Sci. 2014;91(2):163–170. doi:10.1097/OPX.0000000000000134
14. Murphy O, O’ Dwyer V, Lloyd-Mckernan A. The efficacy of warm compresses in the treatment of meibomian gland dysfunction and demodex folliculorum blepharitis. Curr Eye Res. 2020;45(5):563–575. doi:10.1080/02713683.2019.1686153
15. Olafsson J, Lai X, Landsend ECS, et al. TheraPearl eye mask and blephasteam for the treatment of meibomian gland dysfunction: a randomized, comparative clinical trial. Sci Rep. 2021;11(1):22386. doi:10.1038/s41598-021-01899-8
16. García-Marqués JV, Talens-Estarelles C, Martínez-Albert N, et al. Evaluation of the MGDRx eyebag treatment in young and older subjects with dry eye symptoms. J Fr Ophtalmol. 2022;45(1):20–27. doi:10.1016/j.jfo.2021.08.009
17. Wang MT, Jaitley Z, Lord SM, et al. Comparison of self-applied heat therapy for meibomian gland dysfunction. Optom Vis Sci. 2015;92(9):e321–6. doi:10.1097/OPX.0000000000000601
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
