Back to Journals » International Medical Case Reports Journal » Volume 17
Post-Sympathectomy Care in Patients with Incessant Ventricular Tachycardia: A Case Study
Authors Ikawati D , Ganefianty A, Nursiswati N, Rahayu U, Kurniawan T, Pahria T
Received 7 April 2024
Accepted for publication 7 August 2024
Published 13 August 2024 Volume 2024:17 Pages 745—750
DOI https://doi.org/10.2147/IMCRJ.S465570
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Vinay Kumar
Dewi Ikawati,1 Amelia Ganefianty,2 Nursiswati Nursiswati,3 Urip Rahayu,3 Titis Kurniawan,3 Tuti Pahria3
1Master Program of Nursing Universitas Padjadjaran, Bandung, Indonesia; 2Hasan Sadikin Hospital, Guest Lecturer Faculty of Nursing, Universitas Padjadjaran, Bandung, Indonesia; 3Faculty of Nursing, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Nursiswati Nursiswati; Dewi Ikawati, Department Medical-Surgical Nursing, Faculty of Nursing, Universitas Padjadjaran, Citra Graha Handayani, Citra Utama street No. 22, Sumedang, Bandung, 45362, Indonesia, Tel +6281294885959, Email [email protected]; [email protected]
Introduction: Incessant Ventricular Tachycardia is a condition characterized by multiple episodes of Ventricular Tachycardia (VT) in 24 hours, persisting despite efforts to stop the arrhythmia. In this condition, sympathectomy as the surgical procedure is considered a permanent intervention and the last resort when medications prove ineffective. This procedure comprises the cutting or clamping of sympathetic nerves to prevent the transmission of nerve signals. Therefore, this study aims to present a case report of post-sympathectomy nursing management in a patient with Incessant Ventricular Tachycardia.
Case Presentation: A 59-year-old female patient was admitted to the high-care unit with a diagnosis of post-sympathectomy, Incessant Ventricular Tachycardia due to Arrhythmogenic Cardiomyopathy. Nursing problems based on NANDA included decreased cardiac output, gas exchange impairment, and activity intolerance. Furthermore, the nursing interventions for the condition included self-care management and collaboration with an anesthesiologist and cardiologist. The interventions encompassed cardiac care, airway management, and activity therapy. Tele-nursing was also conducted through video calls to monitor the patient after hospital care.
Results: The planned nursing care was effective in preventing common complications that often occur after the surgical procedure. The most important key aspect is regular maintenance and monitoring. The patient was discharged on the third day after the surgery with no complaints of shortness of breath, palpitations, and gradual resumption of activities.
Conclusion: Sympathectomy procedures could successfully be used to treat patients through multidisciplinary collaboration. Furthermore, nurses could emphasize post-operative care management to expedite recovery and improve patient quality of life.
Keywords: sympathectomy, role of nurses, post-operative care
Introduction
Sympathectomy is a surgical procedure comprising the cutting or clamping of sympathetic nerves to interrupt the transmission of nerve signals. Furthermore, this procedure is often considered a permanent intervention and a last resort when medications become ineffective. In patients with heart arrhythmias, sympathectomy is a potential solution for ventricular tachycardia (VT), which remains refractory to clinical treatment and ablation.1 For patients suffering from Incessant Ventricular Tachycardia, prolonged and repetitive VT episodes lasting for hours are typically observed.2 VT storms are characterized by the occurrence of three or more separate episodes in 24 hours, each requiring intervention, with a common complaint of persistent palpitations.3
The success of sympathectomy in heart disease has been proven internationally, with 73% of 22 patients experiencing a significant reduction in arrhythmia, 53% becoming arrhythmia-free, and 27% being unresponsive to treatment.4 According to Ajijola et al, the success rate in suppressing ventricular arrhythmia reached 70%. Despite these promising outcomes abroad, it is important to note that there is currently no definitive source in Indonesia discussing the procedure.5
Several studies showed that sympathectomy had the potential for significant impact and could also lead to complications.6 These complications include neuropathic pain or chronic pain due to damaged nerves caused by the disruption of the sympathetic chain and Horner syndrome.7,8 Other side effects include shortness of breath, heart arrhythmia disturbances or relapses, and the presence of pneumothorax due to residual gas, requiring chest tube drainage.9
Given the possible range of complications, the role of nurses in post-sympathectomy cases becomes crucial10. The engagement of nurses is essential in both preventing potential side effects and addressing patient concerns. The main focus of post-sympathectomy care includes several critical aspects: firstly, monitoring of vital signs such as blood pressure, pulse, respiration and body temperature is done early to detect early signs of complications. Secondly, airway assessment to ensure the patient is well ventilated, which includes checking oxygen saturation, lung auscultation, and respiratory pattern.
Thirdly, neurological status which includes checking the patient’s level of consciousness, muscle strength, changes in mental status, and emotional state. Fourth, pain management assesses pain intensity, pain location, pain characteristics, and pain duration. Fifth, assessment of the condition of the surgical wound by assessing the condition of the wound, whether there are signs of infection, drainage, the condition of the clit around the wound and the installation of drains. Sixth, fluid and electrolyte balance assessment, namely assessing fluid intake and output, hydration status, body weight, signs of fluid overload, and laboratory values. Primary nursing interventions in this case focus on addressing the decrease in cardiac output due to arrhythmia, managing gas exchange issues caused by pneumothorax and promoting suitable activity. This method has been reported to have the ability to improve and enhance patient quality of life.11
Case Presentation
In this case report, the patient gave informed consent to participate and to publish. A 59-year-old married female of Sundanese ethnicity who worked as a housewife. Upon admission to the high-care unit, a diagnosis of post-sympathectomy, namely Incessant Ventricular Tachycardia caused by Arrhythmogenic Cardiomyopathy dd IDCM (Ischemic Dilated Cardiomyopathy), and Chronic Heart Failure, NYHA FC II, was established. The patient had a history of palpitations for the last year and had been receiving tablet therapy at a local clinic, however the patient did not know the name of the medicine he was taking, according to him, he forgot and there were many kinds of medicine he was taking. Despite the intake of regular medication, the symptoms experienced remained persistent. In the two months preceding admission, the condition worsened, manifesting as increased palpitations, irregular heartbeats, shortness of breath, dizziness, and fainting. Consequently, the patient was referred to a specialized hospital and underwent sympathectomy with thoracic sympathetic nerve ablation (T1-T3) using Video Assisted Thoracoscopic Surgery (VATS).
According to the patient, the symptoms experienced in the past two months were caused by emotional distress, characterized by sadness and anxiousness. This was because the eldest child of the patient, who was already married, went through a divorce and developed a mental disorder after the separation. The child’s erratic behavior, wandering around the neighbors’ houses and damaging properties, induced anxiousness, leading to increased palpitations. Examination showed a history of low blood pressure, but no history of hypertension or diabetes mellitus. Furthermore, in the family health history, there were no instances of heart disease or premature death due to heart attack.
During the assessment on the first day after the surgery, there were complaints of shortness of breath, pain in the left chest where the operation was performed, and a general feeling of weakness. Observation showed a blood pressure of 98/61 mmHg, with 22 breath per minute respiratory rate (RR), 61 beats per minute heart rate (HR), 36.5°C temperature, 98% oxygen saturation (SPO2), and 106 mmHg mean arterial pressure (MAP). Furthermore, the pain level was rated as 2 on Numeric Rating Scale (NRS). The patient was conscious and alert, for neurological status using Glasgow Coma Scale (GCS) score of E = 4 M = 6 V = 5. The conjunctiva was not anemic, the sclera was not jaundiced, jugular venous pressure (JVP) was 5+2 cm, the shape and movement of the chest appeared symmetrical, heart sounds S1 and S2 were regular, with no S3 or S4 sounds, murmurs, rales, or wheezing. The abdomen was distended, with bowel sounds heard at 10 times per minute. Acral extremities were warm, capillary refill time (CRT) was less than 2 minutes, and there was no edema. The examination showed the presence of a wound on the chest with chest tube thoracostomy (CTT) measuring 5 cm × 2 cm. The fall risk assessment using the Morse scale showed a high-risk level. The monitoring can be seen in Figures 1–3.
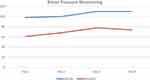 |
Figure 1 Blood pressure monitoring. |
 |
Figure 2 Respiratory, Oxygen saturation, Pulse, Temperature monitoring, Status neurological and Pain management. |
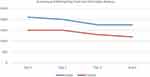 |
Figure 3 Assessing and maintaining fluid and electrolyte balance. |
Electrocardiography (ECG) played a crucial role in the pre- and post-operative assessment. ECG showed a monomorphic Ventricular Tachycardia pattern before the procedure (Figure 4). After the operation (Figure 5), ECG showed sinus rhythm with a prolonged QTc (458ms). Chest X-ray before the operation showed cardiomegaly with no pulmonary congestion. Results before the procedure showed a dilated left ventricle (LV), eccentric left ventricular hypertrophy (LVH) with reduced LV systolic function (LVEF 33%), regional wall abnormalities, and regional right ventricular (RV) wall akinesia. LV diastolic dysfunction was classified as grade I, with normal anatomy and function of all valves. Furthermore, there was a low probability of ventricular hypertrophy (VH) and reduced RV systolic function with regional wall motion abnormalities, meeting the echo major criteria of PADUA score for arrhythmogenic cardiomyopathy. Angiography before the operation showed severely reduced LV systolic function (LVEF 27%). Laboratory results for ion calcium, magnesium, and troponin T before the surgery were within normal limits.
 |
Figure 4 ECG photo of the patient before sympathectomy. |
 |
Figure 5 Photograph of ECG examination after sympathectomy. |
The patient received intravenous treatment with 0.9% NaCl fluid at a rate of 1500 cc per 24 hours, Paracetamol 1 × 1 gram, Omeprazole 2 × 1 gram, oral Cefixime antibiotics 2 × 200 mg, intravenous Vitamin K 3 × 10mg, intravenous Tranexamic Acid 3 × 500mg, and heart medication for arrhythmia, namely Bisoprolol tablet 1 × 2.5 mg (given when HR > 65 beats per minute), and Spironolactone tablet 1 × 25mg (given when mean arterial pressure is between 70 and 100 mmHg).
In terms of Nursing Diagnoses based on North American Nursing Diagnosis Association (NANDA), the priorities identified included 1). Decreased Cardiac Output related to changes in heart rhythm, 2). Impaired Gas Exchange related to an imbalance in ventilation-perfusion, and 3). Activity intolerance related to an imbalance between oxygen supply and demand.12
The selected nursing interventions based on NIC (Nursing Interventions Classification) and NOC (Nursing Outcomes Classification) for the first nursing problem, which was a decrease in cardiac output, emphasized cardiac care management and collaborative administration of medications, such as propranolol and spironolactone. This also comprised the evaluation of chest pain, monitoring fluid balance, changes in blood pressure, mean arterial pressure (MAP), and respiratory status, as well as assisting in reducing anxiety through deep breathing relaxation techniques. Vital sign management was also carried out including monitoring blood pressure, respiratory rate, heart rate, and temperature. The procedures also comprised recording blood pressure changes and monitoring heart sounds.
For the second nursing problem, which was the gas exchange issue, airway management was conducted. This included auscultating breath sounds, recording any additional sounds, and monitoring respiration, oxygen status, CTT hose as well as undulations, and fluid from CTT. The third nursing problem, namely patient activity intolerance, was managed through activity therapy. Continuous evaluation was carried out, and a follow-up was accomplished through a video call. The results showed that with planned nursing care, complications that often occurred after the surgery could be prevented. On the second day post-surgery, there was no complaint of shortness of breath and palpitations. This led to the removal of the chest tube and discharge. Mobilization and activities were performed gradually in this case. Upon discharge, the patient was able to stand and walk around the bed area, with enhanced adaptation to the pain. For the follow-up care evaluation with tele-nursing, a video call was conducted to provide guidance on maintaining activities according to the heart capacity. The patient was pleased to be contacted, had no shortness of breath complaints, and activities had started gradually.
Discussion
In the case of a female patient experiencing post-sympathectomy due to Incessant Ventricular Tachycardia, sympathectomy was performed after a year of oral therapy with no improvement. The increasing severity of the symptoms was triggered by anxiety related to mental health problems regarding the first child of the patient, leading to the decision to undergo operative therapy with sympathectomy.
The classic presentation of Incessant Ventricular Tachycardia included palpitations and irregular heartbeats, EKG showing monomorphic Ventricular Tachycardia, and echocardiography showing a decrease in EF. According to previous studies, the sympathetic nervous system, specifically postganglionic sympathetic fibers from the stellate thoracic ganglia and T2-T4, controlled heart function and played a crucial role in ventricular arrhythmia initiation and maintenance. Although the middle cervical ganglia also provided significant innervation to the heart, the removal of the thoracic ganglia T2-T4 gave sufficient efferent and afferent denervation to treat heart arrhythmias.13
The role of nurses in post-sympathectomy management was focused on preventing complications,14 cardiac care, gas exchange, activity therapy, and evaluation. Furthermore, it was crucial to monitor and maintain cardiac output because increasing stroke volume, parallel to Frank–Starling mechanisms, compensated for decreased heart rate and direct myocardial contractility reductions due to sympathectomy.15 EKG monitoring was performed as recommended by Hofferben to ensure the absence of arrhythmias, such as bradycardia.
Continued evaluation carried out in this study included follow-up care through tele-nursing. Based on previous studies, monitoring should be conducted for up to 6 months and one year, thereby requiring further study to determine the ongoing of patient progress for a more in-depth evaluation.4 This was because bradycardia after sympathectomy was relatively common, with one study showing an average 15% decrease in heart rate within 24 hours, lasting for 6 months.16
Conclusion
In conclusion, sympathectomy was a surgical procedure designed to permanently sever the sympathetic nerve, typically pursued when conventional medical treatments prove ineffective. Furthermore, this procedure was often used among patients suffering from heart disease with Incessant Ventricular Tachycardia. In this case, the role of nurses was to prevent complications through accurate nursing care planning, thereby minimizing the length of stay, expediting patient recovery, and improving the quality of life. The follow-up care program was carried out to identify any complications or the need for further intervention.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pêgo-Fernandes PM. Surgical Sympathectomy: can it be useful in cardiology? Clinics. 2020;75:e1819. doi:10.6061/clinics/2020/e1819
2. Foth C, Gangwani MK, Ahmed I, Alvey H. Ventricular Tachycardia. In: StatPearls. Treasure Island (FL): StatPearls Publishing LLC; 2024.
3. Shenthar J. Unusual incessant ventricular tachycardia: what is the underlying cause and the possible mechanism? Circulation. 2015;8(6):1507–1511. doi:10.1161/CIRCEP.115.002886
4. Hofferberth SC, Cecchin F, Loberman D, Fynn-Thompson F. Left thoracoscopic sympathectomy for cardiac denervation in patients with life-threatening ventricular arrhythmias. J Thoracic Cardiovasc Surg. 2014;147(1):404–409. doi:10.1016/j.jtcvs.2013.07.064
5. Ajijola OA, Vaseghi M, Mahajan A, Shivkumar K. Bilateral cardiac sympathetic denervation: why, who and when? Exp Rev Cardiovasc Therap. 2012;10(8):947–949. doi:10.1586/erc.12.93
6. Afshar H, Rasekh A, Treistman B, Van Leeuwen C, Duncan JM, Massumi A. Cryoablation of incessant ventricular tachycardia: case report and long-term follow-up.. Texas Heart Inst J. 2000;27(1):52–54.
7. Straube S, Derry S, Moore RA, Cole P. Cervico-thoracic or lumbar sympathectomy for neuropathic pain and complex regional pain syndrome. Cochrane Database Syst Rev. 2013;2013(9):Cd002918. doi:10.1002/14651858.CD002918.pub3
8. Study Bedah. Modul 12 Bedah TKV; 2016:1–23.
9. Ovalı C, Sevin MB. Effectiveness, success rates, and complications of different thoracoscopic sympathectomy techniques in patients with palmar hyperhidrosis. Turk Gogus Kalp Dam Cerrah Dergisi. 2018;26(1):86–92. doi:10.5606/tgkdc.dergisi.2018.14686
10. Rosidawati I, Ibrahim K, Nuraeni A. Kualitas Hidup Pasien Pasca Bedah Pintas Arteri Koroner (BPAK). J Keperawat Padjadj. 2017;4(2). doi:10.24198/jkp.v4i2.238
11. Suyanti T, S R. Lama post operasi Coronary Artery Bypass Graft (CABG) dengan kualitas hidup pasien post operasi CABG di RSPAD Gatot Soebroto. J Akadem Baiturrah Jambi. 2020;9(2):166–173.
12. Nurarif AH, H K. Aplikasi asuhan keperawatan berdasarkan diagnosa medis & Nanda NIC-NOC; 2015.
13. Kopecky K, Afzal A, Felius J, et al. Bilateral sympathectomy for treatment of refractory ventricular tachycardia. Pacing Clin Electrophysiol. 2018;41(1):93–95. doi:10.1111/pace.13164
14. Aksu T, Guler TE, Golcuk E, Ozcan KS, Erden I. Ablation of idiopathic ventricular tachycardia originating from posterior mitral annulus by using electroanatomical mapping. Internat Med Case Rep J. 2015;8:71–75. doi:10.2147/IMCRJ.S79519
15. Fiorelli A, Messina G, Chiodini P, et al. Cardiac autonomic changes after thoracic sympathectomy: a prospective, randomized study. Ann Thorac Surg. 2017;103(1):216–224. doi:10.1016/j.athoracsur.2016.10.055
16. Chung JS, Sieunarine K, Deague JA, Hawkins DJ. Asystole following bilateral endoscopic thoracic sympathectomy. Anaesth Intens Care. 2021;49(3):234–236. doi:10.1177/0310057X21992778
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
