Back to Journals » Clinical Ophthalmology » Volume 18
Pre-Cycloplegic Exam Benefit of Photoscreening and Accommodation-Relaxing Skiascopy
Authors Schaafsma JD, Arnold RW
Received 11 December 2023
Accepted for publication 21 February 2024
Published 15 March 2024 Volume 2024:18 Pages 833—846
DOI https://doi.org/10.2147/OPTH.S454430
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract of “Benefit Of Photoscreening And Accommodation-Relaxing Skiascopy” [454430].
Views: 58
Jacob David Schaafsma,1 Robert W Arnold2
1School of Medicine, University of Milan, Milan, Italy; 2Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, Anchorage, AK, USA
Correspondence: Robert W Arnold, Alaska Blind Child Discovery, Alaska Children’s EYE & Strabismus, 3500 Latouche Street #280, Anchorage, AK, 99508, USA, Tel +1(907)561-1917, Fax +1(907)563-5373, Email [email protected]
Background: Seeking a quick way to estimate refractions for challenging pediatric patients, we studied two non-contact methods with particular attention to accuracy and level of stress in uncovering cycloplegic hyperopia.
Methods: Newly referred and follow-up pediatric eye patients had timed school bus accommodation-relaxing skiascopy (SBARS) and Plusoptix A12 (Px) photoscreener testing before cyclopentolate 1% confirmatory examinations. The ABCD ellipsoid univariate method based on relative blur and vector components was used to compare dry sphero-cylinder refraction estimates with cycloplegic. Receiver operating characteristic (ROC) curves were used to determine screening value.
Results: Three compared refractions were attempted in 191 racially diverse children of whom 100 were age 0.2– 3.9 years and 91 were 4 to 14 years. Plusoptix failed to yield a result in 21 and an additional 21 were interpreted as an excess sphere. Median spherical equivalent did not differ between Px and SBARS for 149 with Px readings but in hyperopic patients, Plusoptix uncovered 27% less hyperopia. The ellipsoid for SBARS of 0.8 was better than 2.4 for Plusoptix (Mann–Whitney p< 0.001). Plusoptix was fastest (3– 15 seconds) followed by SBARS (15– 30 seconds) compared to 30– 45 minutes for cycloplegic exam.
Conclusion: Non-contact quick refractive methods enhanced confirmatory cycloplegic pediatric exam in high-risk pediatric patients.
Keywords: sphero-cylinder, refraction, autorefraction, photoscreening, developmental delay
Introduction
Refraction in the pediatric eye examination is critically important but can be difficult, stressful and slow.1 Perhaps, some modern screening techniques could be useful as a part of a confirmatory pediatric eye examination. Two non-contact techniques that can be useful in community screening for amblyopia could also be utilized as an early aspect of a confirmatory eye examination. They are dry retinoscopy and infrared multi-radial photoscreening. Dr David Silbert, who also continues to value the advantages of photoscreening as a component of pediatric eye exams, tried to answer whether a leading photoscreener could replace cycloplegic examination.2 A question remains: How useful are these non-contact techniques in the eye exam of high-risk pediatric patients?
Retinoscopy with or without enhancements such as dynamic retinoscopy or skiascopy can serve as a helpful vision screening tool. Eibschitz proved localized community amblyopia reduction when a group of plus-3 retinoscopy-screened children then treated were compared to a local, age-matched community cohort.3 The NIH-sponsored phase-1 of the Vision in Preschoolers (VIPS) study evaluated experienced-optometrist-retinoscopy (non-cycloplegic retinoscopy) which out-performed early photoscreeners, hand-held autorefractors and visual acuity in terms of sensitivity to detect amblyopia risk factors.4 Dynamic retinoscopy has value in estimating accommodative reserve or compromise as a risk for amblyopia in children who can thus cooperate.5 The dynamic response to skiametry further enhances the evaluation of hyperopia and latent hyperopia.6
Photoscreening employs pupillary red reflex evaluation with a nearly coaxial light source such that crescents of light appear as a function of refractive error in various merida.7,8 More than two decades ago, photoscreening was practically employed by Angi and Freedman to detect amblyopia.9,10
Hyperopia in one or more meridia, in one or both eyes, is a predominant amblyopia risk factor.11 Moderate hyperopia detected during cycloplegic retinoscopy is common and normal in most young children. On the other hand, excess hyperopia for which accommodation is not sufficient can cause refractive amblyopia, or if accommodation is excessive can cause accommodative esotropia leading to strabismic amblyopia. The type of fixation target on a photoscreener can regulate the degree of accommodation and uncover higher degrees of potentially amblyopiagenic, latent hyperopia.12
Photoscreeners are designed to be used in the pediatric medical home, or community outreach, to uncover children with excess amblyopia risk factors. We studied how photoscreeners can also have a helpful role used in the pediatric ophthalmologist office providing refractive and ocular alignment estimates before and after cycloplegia.
Self-adjusted spherical spectacles have value in predicting refraction, however they can underestimate hyperopia due to allowed accommodation.13 In fact, visual acuity by dry automated refraction outperformed cycloplegic visual acuity in this recent study.
Spectacle prescriptions can be mathematically compared. The gold-standard method involves converting the three sphero-cylinder components sphere, cylinder magnitude and cylinder axis via vector transformation into a spherical equivalent and the two J0 and J45 components.14 These two J0 and J45 vectors can then be further converted 3-dimensionally and compared on the basis of relative spectacle blur and age to derive an “ellipsoid” univariate metric for spectacle comparison.15 Using the ellipsoid method, a smaller value of 1.0 or less indicates that the candidate spectacle will yield visual acuity within one logMAR line of the ideal target spectacle.15 An ellipsoid value of 2.0 means the candidate spectacle yields visual acuity blur of 3 lines from ideal target and an ellipsoid value of 3.0 or more yields a visual acuity blur within 6 or more logMAR lines.16
Reducing or blocking accommodation has been needed to reveal the actual amount of hyperopia. Cycloplegia is the gold-standard method for reducing accommodation. However, there are practical difficulties with cycloplegia including pain and stress with the eye drops, wash-out due to reflex lacrimation and imperfect absorption of the drop. Another method for reducing accommodation is fogging by placing a higher plus lens over the non-retinoscoped eye.17 If a rack of plus lenses are held vertically over the retinoscoped eye, hyperopia may be missed.18 On the other hand, a specially crafted plus lens rack held horizontally over both eyes has the potential to uncover much more hyperopia even without cycloplegia as long as the child is willing to participate.19
Methods
This prospective evaluation of screening tests is undertaken by the Alaska Blind Child Discovery research project and complies with the Declaration of Helsinki and the Health Insurance Portability and Accessibility Act (HIPAA) with Institutional Review by Providence Alaska Medical Center. Parents and/or guardians gave written informed consent and patients with developmental age older than 13 years also gave written assent. De-identified data can be retrieved from https://www.abcd-vision.org/references/SBARS%20PX%20De-ID%202023.pdf.
New patients referred by pediatric and community photoscreening and therefore at high risk for amblyopic refractive error and follow-up pediatric ophthalmology patients already accustomed to spectacles were recruited for this study. At the onset of the examination, before any cycloplegia, experienced staff performed Plusoptix A12 (Px) photoscreening and also estimated refractive error using the school bus accommodation-relaxing skiascopy (SBARS: Eye Care and Cure – Hilco, Phoenix, Az;) technique. A Plusoptix A12 (software version 7.2.5.0) remote autorefraction was attempted on all patients. The Plusoptix manufacturer suggests a capability to estimate refractions between −7 D and +5 D. When the device interprets excess myopia sphere or cylinder, it reports “MYO” and for excess spherical or cylinder hyperopia reports “HYP”. For numeric calculations, we substituted a refractive value of −7.00 sphere for all reports of “MYO” and a value of +5.00 sphere for all reports of “HYP”. When the Plusoptix was unable to give an estimate due to small or indeterminate pupils, or fixation loss or constant strabismus, those cases were analyzed as a “Plusoptix No-Read”.
Then, the remainder of the confirmatory examination was performed including age-appropriate estimation of visual acuity and ocular motility before 1% cyclopentolate cycloplegia. To numerically account for visual acuity in young children, we employed a fixation-based logMAR estimate.20 Thirty minutes later the exam was completed with cycloplegic retinoscopy which was then refined at the phoropter in cooperative patients and finally the ocular media and retinae were examined. Determination of any prior refraction and review of chart history was completed after the initial Plusoptix photoscreening and dry SBARS retinoscopy. Data were collected on patient age, gender, race/ethnicity and whether a developmental delay was present.
Patient cooperation with pediatric refraction and eye examination can be very challenging. The level of patient cooperation during SBARS and PlusoptiX was defined as follows: good – gazes through lenses or at photoscreener for several seconds each higher plus, fair – will briefly glance and allow some increase in plus but still might be crying or upset, and poor: too timid or crying and will not voluntarily gaze through SBARS lenses or at the photoscreener fixation target. The times to estimate and then confirm refractive error were measured. Level of cooperation and time for exam are presented in Table 1.
Sample Size Calculation
For mean value refractive error of 1.0 and standard deviation of 2.0, the alpha of 5% and power of 0.8, the sample size to detect a 0.25 diopter difference is 63. If only about 1/3 have good cooperation and have readings on Plusoptix, then at least three times 63 or 189 patients is needed.
Spectacle Refraction Comparison
A single numeric grade for matching two spectacles relative to achievable visual acuity and age-appropriate accommodation called the ABCD Ellipsoid was used to determine how well each dry (before cycloplegia) refraction estimation technique (SBARS and Plusoptix) compared with the immediately subsequent, same-day, same-hour cycloplegic retinoscopy with phoropter refinement when possible. Cycloplegia was achieved with one drop of cyclopentolate 1% and waiting at least 30 minutes.
Seeking to assess the ability to uncover hyperopia, we defined refractive divisions in different ways depending on the comparison. Emmetropia for these children was defined between −1.00 myopic and +0.75 hyperopic cut-offs. Hyperopia was a spherical equivalent greater than or equal to +0.75 and myopia was a spherical equivalent/lowest meridian less diopter power or equal to −1.00- magnitude of myopic meridian equal to or more than 1 diopter. To increase the cohort, “all hyperopia” of all patients expected to require some accommodation for distance and near viewing, patients were defined as those with cycloplegic spherical equivalent greater to 0.0 D. We defined those patients with astigmatism as a magnitude of astigmatism greater than or equal to 1.50 diopters.
Amblyopia Risk Factor Screening
For vision screening performance of the SBARS and Plusoptix, we employed the age-based 2021 AAPOS Uniform amblyopia risk factor failure levels.11
The normality of the data was assessed by Shapiro–Wilk test. When data was found to not be normally distributed, non-parametric tests (Mann–Whitney and Kruskal–Wallis) were employed. For proportions, Chi-square was used. Bland-Altman analysis following intra-class correlation was used to compare two tests applied to each identical, continuous data set.
Results
Confirmatory eye examinations that included pre-cycloplegic photoscreening attempt and School Bus Accommodation Relaxing Skiascopy (SBARS) were performed on 191 children. In addition, infrared, multi-radial on-site interpreted photorefraction was done with a Plusoptix A12 before cycloplegia. Characteristics of the patients are summarized in Table 2. Ages ranged from 0.2 to 14.6 years with 100 under age 4 years and 91 children 4 years and older. There were 84 females and a racial/ethnic mix of 17 Black, 17 Alaska Native, 19 Hispanic White, 27 Pacific Islander, 31 Asian and 80 non-Hispanic White. There were 43 patients with developmental delay including 14 ex-premature, 13 with autism, 6 with Down or other syndromes, and 4 with structural central nervous system defects. Ninety-five were referred from photoscreening at their pediatrician’s office visit or from school photoscreening clinics. Twenty-one had no reading from Plusoptix A12, while another 21 had excess values in at least one eye; 4 were interpreted as MYO for excessive myopia and 7 were HYP for excessive hyperopia right eye while for the left eye 2 were MYO and 15 were HYP interpreted excesses. For all patients right and left eyes, visual acuity median was 20/41 (IQR1 20/32, IQR3 20/41).
 |
Table 2 Patient Characteristics |
The level of cooperation with refractive estimates was poor in 19, fair in 77 and 113 cried and resisted with cycloplegia (Table 1). Cycloplegic examination took 30–45 minutes while SBARS took 20–30 seconds and Plusoptix 3–15 seconds to yield a sphero-cylinder refraction in both eyes.
Spectacle Refraction Comparison
Table 3 shows values for spherical equivalent and for ellipsoid comparing candidate SBARS and Plusoptix refraction estimates and the target cycloplegic refractions. The distributions of ellipsoid and spherical equivalent for cycloplegic exams, for SBARS and for Plusoptix were found to not be normally distributed by Shapiro–Wilk test, therefore non-parametric analysis using medians and interquartile ranges (IQR1, IQR3), and Mann–Whitney and Kruskal–Wallis were used for comparative analysis. For all the 170 patients with Plusoptix readings, the spherical equivalent showed no difference between cycloplegic exam, Plusoptix and SBARS by Kruskal–Wallis for right eyes (X2(2) = 5.6, p=0.06) or for left eyes (X2(2) = 3.1, p=0.21).
 |
Table 3 Ellipsoids, Spherical Equivalents and Cylinder Predictions |
Figure 1 shows Bland Altman analysis of spherical equivalent when candidates SBARS and Plusoptix targeted cycloplegic exam. For all patients with Plusoptix readings and any spherical equivalent hyperopic cycloplegic refraction >0D, the 130 median (IQR1, IQR3) right eye cycloplegic, Plusoptix and SBARS spherical equivalents were +1.37D (+0.75D, +2.25D), +1.00D (+0.37D, +1.88D) and +1.13D (+0.38D, +1.75D), respectively. The corresponding 132 left eye refractive values were cycloplegic +1.38D (+0.75D, +2.38D), Plusoptix +0.88D (+0.38D, +2.00D) and SBARS +1.00D (+0.50D, +2.00D). The Plusoptix estimates accounted for a median 75% (IQR 19%, 150%) of the 130 true right eye cycloplegic hyperopia while SBARS accounted for 91% (IQR 67%, 111%). For the 132 hyperopic left eyes, Plusoptix accounted for 71% (IQR 17%, 125%) and SBARS 90% (IQR 63%, 108%).
The spherical equivalent for the 130 right eyes with SBARS median +1.06 compared to Plusoptix +1.00 (Mann–Whitney z=1.97, p=0.5) while the 132 hyperopic left eyes median SBARS +1.0 did not differ from Plusoptix +0.88 (Mann–Whitney z=1.06, p=0.30). The difference between cycloplegic refraction and the estimation techniques was evaluated for hyperopic cases: from 130 right eyes. SBARS median of 0.90 differed from the 130 right eye Plusoptix 0.74 (Mann–Whitney z=2.04, p=0.4), but for left eye the SBARS median of 0.98 did not differ from 132 left eye Plusoptix median of 0.75 (Mann–Whitney 0.31, p=0.760).
For the Plusoptix refraction-capable and hyperopic patients, the percent predicted hyperopia comparing SBARS and Plusoptix targeting cycloplegic exam right eyes (91% vs 70%; Mann–Whitney z=2.6, p=0.009) and left eyes (96% vs 54%, Mann–Whitney z=1.7, p=0.097) showed unequal medians comparing both eyes (Kruskal–Wallis X2(3) = 9.4, p=0.025). For the hyperopic patients with Plusoptix readings, over minus by more than 1 diopter 124 right eyes were 11% for SBARS and 31% for Plusoptix (Chi-square z=3.7, p<0.001) and for 117 left eyes 13% SBARS and 33% Plusoptix (Chi-square z=3.6, p<0.001). The visual acuity for patients who had a result with Plusoptix differed and was better than for children who did not have a Plusoptix result (Mann–Whitney z=3.9 right eyes, and 2.4 left eyes, p<0.001 and p=0.02).
Figure 2 and Table 4 highlight the Bland Altman analysis of ellipsoid spectacle image resolution grade comparing the ability of SBARS and of Plusoptix to target cycloplegic exam. For the 130 right eye hyperopic patients, ellipsoid for the Plusoptix 2.38 was greater than for SBARS 0.90 (Mann–Whitney z=8.2, p<0.001) and for the 132 left eyes Plusoptix 2.49 differed from SBARS 0.72 (Mann–Whitney z=9.0, p<0.001).
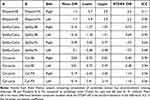 |
Table 4 Bland Altman Analysis |
The Ellipsoid for all 170 completed Plusoptix of median 2.33 differed from the corresponding estimates by SBARS right eyes 0.80 (Mann–Whitney z=9.6, p<0.001). For left eyes, Plusoptix estimates 2.30 differed from SBARS 0.80 (Mann–Whitney z=9.5, p<0.001).
The interactions and comparisons of factors influencing ellipsoid and refractive components are summarized in Table 5. There was a significant 2-way ANOVA interaction based on developmental delay combined with level of cooperation on right SBARS ellipsoid (F(2164) = 3.5, p=0.03) but not for left SBARS ellipsoid (F(2164) = 1.7, p=0.18). There was no interaction combining developmental delays and level of cooperation for Plusoptix right ellipsoid (F (2164) = 1.5, p=0.22) and for left eye (F(2164) F(2164) = 0.93, p=0.39). By Kruskal–Wallis, there was no difference in SBARS ellipsoid by race for right eyes (X2(7) = 8.1, p=0.32) and left eyes (X2(7) = 5.7, p=0.57). By Kruskal–Wallis, the median SBARS ellipsoid did not differ by spherical equivalent refractive error designation (hyperopia > 0.75D myopia <1.0D and emmetropia in between) for ellipsoid right eyes (X2(2) = 2.5, p=0.29) and left eyes (X2(2) = 4.3, p=0.12).
 |
Table 5 Compared Influences on SBARS and Plusoptix Targeting Cycloplegic Refraction |
The influence of new photoscreen referral versus long-term spectacle follow-up exams is shown in Table 6. The new photoscreen refer have never worn spectacles and many suffer from excess hyperopia, whereas the return patients have been accustomed to wearing spectacles that therapeutically compensate for excess hyperopia. There was no significant difference in ellipsoid or spherical equivalent based on prior wearing of spectacles in this high-risk cohort. The new patients with Plusoptix results directly referred by photoscreening (n=85 of the total 95) were compared to an equal number of follow-up patients (n=85) many of whom were already wearing spectacles. There was no difference in median values of ellipsoid right or left eye for SBARS or Plusoptix based on new referral or follow-up patients already in spectacles (Mann–Whitney z between 0.18 and 1.19, p value from 0.24 to 0.89). There was also no difference in median spherical equivalent right or left eye for cycloplegic exam, SBARS or Plusoptix relative to new referral or follow-up exam status (Mann–Whitney z between 0.03 and 1.1, p value from 0.27 to 0.98).
 |
Table 6 Comparisons of NEW Photoscreen Referral versus RETURN Spectacle Visit Status |
The influence on sub-components of the ellipsoid, J45 vector and M spherical equivalent is shown in Table 7 for SBARS and Plusoptix targeting cycloplegic exam. There was more influence of spherical equivalent than the astigmatic aspect of J45 vector separating SBARS performance compared to Plusoptix.
 |
Table 7 J45 and M Components of Ellipsoids Compared |
Regarding the influence of Plusoptix non-readability cases, the ellipsoid for SBARS corresponding to the 20 Plusoptix non-read right eye median of 1.05 did not differ from those with 170 with PlusoptiX read 0.80 (Mann–Whitney z=0.32, p=0.75) and the left eye non-read median 1.07 versus reads 0.70 (Mann–Whitney z=0.56, p=0.58).
Amblyopia Risk Factor Screening
Figure 3 shows the receiver operating characteristic (ROC) curves screening by Plusoptix A12 and SBARS for age-based 2021 AAPOS amblyopia risk factors.11 AAPOS 2021 amblyopia risk factor sensitivity/specificity for Plusoptix under age 4 years was 84%/74% while for over age 4 years 93%/76%. The corresponding sensitivity/specificity values for SBARS for under 4 years were 68%/94% and for over 4 years 90%/92%.
There were additional benefits of pre-cycloplegic screening. The invisible infrared aspect of Plusoptix photoscreening can be very valuable for certain patients. The device gives a high-quality image of the red reflex showing features such as pupil anomalies like Horner’s syndrome with dark irides, media opacity and lens dislocation (Figure 4). For patients with intense photophobia, the infrared imaging may allow red reflex exam otherwise impossible without examination under anesthesia. The real-time gradual response to SBARS presenting an increasing plus lens over the non-streaked eye yields information on the facility to accommodate for that patient.
Discussion
Non-contact, non-cycloplegic estimates of refractive error were judged in terms of the degree of hyperopia uncovered and by the ability to provide an optically similar spectacle. In a clinical situation with challenging, high-risk children for whom issues of time or cooperation limit the completion of the intended cycloplegic refraction, how reliable would pre-cycloplegic methods be? Both SBARS and Plusoptix performed well. SBARS was a bit more accurate, with more hyperopia uncovered and less over-minus prescription estimates. In this high-risk population, Plusoptix was quicker, but had more un-readable results (21 of 191) and an additional 21 (11 right eyes and 17 left eyes) interpreted as excess hyperopia or myopia.
The good vision screening ROC performance on these high-risk patients resembled the similar performance when selecting the instrument referral criteria for the three major infrared photoscreeners.21 To date, very few studies have addressed the recent 2021 AAPOS amblyopia risk factor definitions,11,22,23 especially for children less than 4 years of age. Plusoptix is a quick, efficient infrared interpreted photoscreener capable of providing an accurate sphero-cylinder refraction with accommodation well controlled in most patients. The infrared image from Plusoptix can also yield clinically helpful information about the red reflex even in otherwise photophobic patients. SBARS is also non-contact but requires nearer proximity to the patient’s face. SBARS is capable of uncovering more than 90% of cycloplegic hyperopia and provides a high-grade estimate of cycloplegic refraction. By adjusting the working distance with the ten convex lenses of SBARS, the single rack substitutes for a whole drawer of loose lenses in an easily carried tool.
Cycloplegia is intended to uncover hyperopia indeed remaining the gold-standard for uncovering hyperopia, but in some patients, it can disrupt cooperation for retinoscopy due to prolonged memory of the painful instillation process. Atropine can uncover more hyperopia than cyclopentolate,24 especially when provided on a daily basis, but may require a return visit. Both Plusoptix and SBARS uncovered much hyperopia, with SBARS uncovering more (93% even in these high-risk patients). Plusoptix uses a large smiley face and sound to elicit fixation and focus, whereas different fixation targets can trigger more or less accommodation from photoscreening devices.12 SBARS utilizes the principle of fogging25–27 to uncover hyperopia and since the bus is held horizontally, uncovers more hyperopia than a vertically held lens rack18 and exceeding the cycloplegic benefit of tropicamide versus cyclopentolate.28
Prior use and familiarity with spectacles might alter a child’s customary level of accommodation, however we found the degree of spherical equivalent and the estimate of spectacle optical precision to be similar whether patients were new photoscreen referrals versus those patients with months to years of spectacle use.
Accurate, quick and child-friendly refraction remains complicated, especially in high-risk pediatric patients who are either too young to cooperate with table-top autorefractors, or who have developmental delays. The Nidek Handy Ref-K at 5 cm uncovered less hyperopia in children than the Welch Allyn SPOT aimed from 100 cm.29 The Grand Seiko open autorefractor and the Topcon KR800 devices were fairly helpful in school-aged Chinese children.30 A brief evaluation suggested that the new QuickSee handheld autorefractor was useful in children with or without cycloplegia.31 Plusoptix performed nearly as well as the hand-held autorefractor Retinomax with32,33 or without34–36 cycloplegia and can be helpful, but young or developmentally challenged children might not participate with steady fixation given the close proximity required by the device. In a previous study, grade B or better spectacle match was achieved by 41% of Plusoptix and 65% for Retinomax.15 SBARS also has a school bus with windows near to the child’s face but is often less stressful and better tolerated by children. Some young children initially fixate on the printed diopter labels adjacent to the SBARS windows but can view through the convex lenses with encouragement. We found 93% of SBARS achieved grade B or better. We had approximately 10% poor cooperation some with Plusoptix, some with SBARS and some with both dry methods, but about 60% were upset with the instillation of cycloplegic drops. Plusoptix usually gives a rapid sphero-cylinder result in children with minimal refractive error. On the other hand, in this high-risk population approximately 10% could not yield a Plusoptix result, and another 10% were interpreted as having excess myopia (MYO) or excess hyperopia (HYP) without a specific sphero-cylinder designation. For this reason, photoscreening clinics should be encouraged to refer patients with a “no result” yield from the Plusoptix.
Conclusion
Though designed to be utilized in pediatric and community-based lay screening, the Plusoptix autorefractor in the pediatric eye specialty clinic provides good estimation of gold-standard cycloplegic refraction with a 30% under-estimation of full hyperopia by as much as 1.5 diopters. The SBARS technique provided excellent estimation of cycloplegic refractive error and uncovered more than 92% of cycloplegic hyperopia. Both techniques are quick, non-contact and generally well tolerated by children, and they both screen well for amblyopia risk factors but require some experience, especially with young, uncooperative, and developmentally delayed patients.
Precis: Non-contact photoscreening designed to be used in the pediatrician environment was tested in an eye clinic with high-risk pediatric eye patients along with horizontally held, convex skiascopy. Both dry methods provided helpful, quick estimates of sphero-cylinder refraction, with Plusoptix having more un-readable and a bit less accurate spectacles compared to cycloplegic confirmatory exams.
Abbreviations
AAPOS, American Association for Pediatric Ophthalmology and Strabismus; ABCD, Alaska Blind child Discovery charitable research Project; ABCD ellipsoid, univariate metric for similarity of two sphero-cylinder refractions based on relative blur of the candidate compared to the target; ANOVA, analysis of variance; Cyl, cylinder measure of astigmatism; D, diopter; HIPAA, Health Insurance portability and Accessibility Act; HYP, Plusoptix interpretation of high hyperopia greater than +5 diopters.; ICC, intraclass correlation coefficient; IQR, inter-quartile range; IQR1 is first and IQR3 is third; J0, sphero-cylinder spectacle vector transform Cartesian component; J45, sphero-cylinder spectacle vector transform oblique component; K-W, Kruskal–Wallis; logMAR, logarithm of the minimum angle of resolution; M; spherical equivalent; Mean Diff, Bland Altman mean different between matched data pairs.; MYO; Plusoptix interpretation of high myopia beyond -7 diopters; M-W, Mann–Whitney; OD, oculo dexter – right eye; OS, óculo sinister – left eye; P, probability; Px, Plusoptix A12 model of photoscreener; Px read, Plusoptix screening that gives either sphero-cylinder or excess sphere interpretation; Px Rx, Plusoptix screening that yields a sphero-cylinder result; ROC, receiver operating characteristic; SB, school bus; SBARS, school bus accommodation-relaxing skiascopy; SphEq, spherical equivalent; STDEV Diff, standard deviation of the difference of each Bland Altman data pair; VIPS, vision in preschoolers study.
Data Sharing Statement
https://www.abcd-vision.org/references/SBARS%20PX%20De-ID%202023.pdf.
Disclosure
Dr Arnold coordinates the Alaska Blind Child Discovery, which has received discounted vision screening technology from several vendors. Dr Arnold is a board member of PDI Check, LLC; consultant for Neolight, outside the submitted work. In addition, Dr Arnold has a patent “Systems and Methods for Eye Evaluation and Treatment” issued. The authors report no other conflicts of interest in this work.
References
1. Wallace DK, Morse CL, Melia M, et al. Pediatric eye evaluations preferred practice pattern(R): I. Vision Screening in the Primary Care and Community Setting; II. Comprehensive Ophthalmic Examination. Ophthalmology. 2018;125(1):P184–P227.
2. Silbert DI, Matta NS, Andersen K. Plusoptix photoscreening may replace cycloplegic examination in select pediatric ophthalmology patients. J AAPOS. 2013;17(2):163–165. doi:10.1016/j.jaapos.2012.11.008
3. Eibschitz-Tsimhoni M, Friedman T, Naor J, Eibschitz N, Friedman Z. Early screening for amblyogenic risk factors lowers the prevalence and severity of amblyopia. J AAPOS. 2000;4(4):194–199. doi:10.1067/mpa.2000.105274
4. VIPS. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the vision in preschoolers study. Ophthalmology. 2004;111(4):637–650. doi:10.1016/j.ophtha.2004.01.022
5. Guyton DL, O’Connor GM. Dynamic retinoscopy. Curr Opin Ophthalmol. 1991;2(1):78–80. doi:10.1097/00055735-199102000-00012
6. Borish IM. Dynamic Skiametry. In: Borish IM, editor. Clinical Refraction.
7. Bobier WR, Braddick OJ. Eccentric photorefraction: optical analysis and empirical measures. Am J Optom Physiol Opt. 1985;62(9):614–620. doi:10.1097/00006324-198509000-00006
8. Kaakinen K. Simultaneous two flash static photoskiascopy. A simple method for screening of children with strabismus or high refractive errors by simultaneous static photographic skiascopy of the horizontal and vertical Meridian of both eyes and the documentation of the corneal and fundus reflexes in one photograph. Acta Ophthalmol. 1981;59(3):378–386.
9. Freedman H, Preston K. Polaroid photoscreening for amblyogenic factors. An improved technology. Ophthalmol. 1992;99(12):1785–1795. doi:10.1016/S0161-6420(92)31722-1
10. Angi MR, Pucci V, Forattini F, Formentin PA. Results of photorefractometric screening for amblyogenic defects in children aged 20 months. Behav Brain Res. 1992;49(1):91–97. doi:10.1016/S0166-4328(05)80198-6
11. Arnold RW, Donahue SP, Silbert DI, et al. Uniform guidelines for pediatric vision screen validation 2021. J AAPOS. 2022;26(1):1.e1–1.e6. doi:10.1016/j.jaapos.2021.09.009
12. Levitt AH, Martin SJ, Arnold RW. Performance of glow-fixation GCK and 2WIN photoscreeners and Retinomax to uncover hyperopia. Clin Ophthalmol. 2020;14:2237–2244. doi:10.2147/OPTH.S256991
13. Zhao L, Wen Q, Nasrazadani D, et al. Refractive accuracy and visual outcome by self-refraction using adjustable-focus spectacles in young children: a randomized clinical trial. JAMA Ophthalmol. 2023;141(9):853–860. doi:10.1001/jamaophthalmol.2023.3508
14. Miller JM. Clinical applications of power vectors. Optom Vis Sci. 2009;86(6):599–602. doi:10.1097/OPX.0b013e3181a6a211
15. Arnold R, Martin SJ, Beveridge JR, et al. Ellipsoid spectacle comparison of PlusoptiX, Retinomax and 2WIN autorefractors. Clin Ophthalmol. 2021;15:3637–3648. doi:10.2147/OPTH.S326680
16. Arnold RW, Beveridge JS, Martin SJ, Beveridge NR, Metzger EJ, Smith KA. Grading sphero-cylinder spectacle similarity. Clin Optom. 2021;13:23–32. doi:10.2147/OPTO.S289770
17. Chiu NN, Rosenfield M, Wong LC. Effect of contralateral fog during refractive error assessment. J Am Optom Assoc. 1997;68(5):305–308.
18. Bigsby W, Gruber J, Rosner J. Static retinoscopy results with and without a fogging lens over the non-tested eye. Am J Optom Physiol Opt. 1984;61(12):769–770. doi:10.1097/00006324-198412000-00012
19. Arnold AW, Arnold SL, Sprano JH, Arnold RW. School bus accommodation-relaxing skiascopy. Clin Ophthalmol. 2019;13:1841–1851. doi:10.2147/OPTH.S219031
20. Arnold RW. Digital values for alpha acuities. JPOS. 2021;58(2):132–135. doi:10.3928/01913913-20210111-02
21. Arnold RW, Silbert DI, Modjesky H. Instrument referral criteria for Plusoptix, SPOT and 2WIN targeting 2021 AAPOS guidelines. Clin Ophthalmol. 2022;16:489–505. doi:10.2147/OPTH.S342666
22. Donahue SP, Arthur B, Neely DE, Arnold RW, Silbert D, Ruben JB. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013;17(1):4–8. doi:10.1016/j.jaapos.2012.09.012
23. Donahue S, Arnold R, Ruben JB. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results from studies of preschool vision screening. J AAPOS. 2003;7(5):314–316. doi:10.1016/S1091-8531(03)00182-4
24. Rosenbaum AL, Bateman JB, Bremer DL, Liu PY. Cycloplegic refraction in esotropic children. Cyclopentolate versus atropine. Ophthalmology. 1981;88(10):1031–1034. doi:10.1016/S0161-6420(81)80032-2
25. Turull-Mallofre A, Garcia-Guerra CE, Mestre C, Vilaseca M, Pujol J, Aldaba M. Influence of power and the time of application of fogging lenses on accommodation. Biomed Opt Express. 2023;14(10):5488–5498. doi:10.1364/BOE.486442
26. Musa MJ, Zeppieri M. Principles and technique of fogging during subjective refraction. In: StatPearls. StatPearls Publishing; 2023.
27. Esteves Leandro J, Meira J, Ferreira CS, et al. Adequacy of the fogging test in the detection of clinically significant hyperopia in school-aged children. J Ophthalmol. 2019;2019:3267151. doi:10.1155/2019/3267151
28. Al-Thawabieh W, Al-Omari R, Abu-Hassan DW, Abuawwad MT, Al-Awadhi A, Abu Serhan H. Tropicamide versus cyclopentolate for cycloplegic refraction in pediatric patients with brown irides: a randomized clinical trial. Am J Ophthalmol. 2023;257:218–226. doi:10.1016/j.ajo.2023.09.022
29. Kizilay O, Akarsu Acar OP, Celik G. İki Farklı El Tipi Taşınabilir Otorefraktometre ile Pediatrik Yaş Grubunda Yapılan Sikloplejili ve Sikloplejisiz Refraksiyon Ölçümlerinin Karşılaştırılması: kesitsel, Gözlemsel Araştırma [Comparison of noncycloplegic and cycloplegic refraction measurements in pediatric patients obtained with two different hand-held portable autorefractometers: cross-sectional, observational research]. Turkiye Klinikleri J Ophthalmol. 2024;33(1):15–21. Turkish.
30. Wang D, Jin N, Pei RX, et al. Comparison between two autorefractor performances in large scale vision screening in Chinese school age children. Int J Ophthalmol. 2020;13(10):1660–1666. doi:10.18240/ijo.2020.10.22
31. Gil A, Hernandez CS, Perez-Merino P, et al. Assessment of the QuickSee wavefront autorefractor for characterizing refractive errors in school-age children. PLoS One. 2020;15(10):e0240933. doi:10.1371/journal.pone.0240933
32. Racano E, Alessi S, Pertile R. Comparison of 2Win and plusoptiX A12R refractometers with Retinomax handheld autorefractor keratometer. J AAPOS. 2019;23(5):276 e1–276 e5. doi:10.1016/j.jaapos.2019.05.017
33. Fledelius HC, Bangsgaard R, Slidsborg C, laCour M. The usefulness of the Retinomax autorefractor for childhood screening validated against a Danish preterm cohort examined at the age of 4 years. Eye. 2015;29(6):742–747. doi:10.1038/eye.2015.14
34. Maguire MG, Ying GS, Ciner EB, et al. Detection of significant hyperopia in preschool children using two automated vision screeners. Optom Vis Sci. 2022;99(2):114–120. doi:10.1097/OPX.0000000000001837
35. Kinori M, Molina I, Hernandez EO, et al. The PlusoptiX photoscreener and the retinomax autorefractor as community-based screening devices for preschool children. Curr Eye Res. 2018;43(5):1–5.
36. Lowry EA, de Alba Campomanes AG. Efficient referral thresholds in autorefraction-based preschool screening. Am J Ophthalmol. 2015;159(6):1180–1187 e3. doi:10.1016/j.ajo.2015.02.012
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





