Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Prevalence and Related Factors of Thyroid Nodules in Physical Examination Population in a Level-A Hospital in Jinan
Authors Meng C, Yang P, Wang Y, Liu S, Wu X, Wang S
Received 7 November 2023
Accepted for publication 22 May 2024
Published 2 August 2024 Volume 2024:17 Pages 3753—3762
DOI https://doi.org/10.2147/JMDH.S443884
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chao Meng,1 Ping Yang,2 Yanan Wang,3 Siyan Liu,3 Xueyan Wu,3 Shaolian Wang3
1Department of General Medicine, Central Hospital Affiliated to Shandong First Medical University, Jinan, People’s Republic of China; 2Department of Integrated Chinese and Western Medicine, Central Hospital Affiliated to Shandong First Medical University, Jinan, People’s Republic of China; 3Department of Endocrinology, Central Hospital Affiliated to Shandong First Medical University, Jinan, People’s Republic of China
Correspondence: Shaolian Wang, Email [email protected]
Background: To investigate the prevalence of thyroid nodules among medical staff and health check-up population in a Level-A hospital (Primary-level hospital) in Jinan City and analyze its influencing factors.
Methods: A total of 5812 cases from the two groups were screened. t-test and χ2 tests were used to analyze the differences in the prevalence of thyroid nodules. Multivariate Logistic regression analysis was used to explore the influencing factors.
Results: The average age of medical staff was (36.20± 9.11) years old, and the total prevalence was 48.5%. The average age of the healthcare population was (57.89± 12.51) years old, and the total prevalence rate was 63.9%, with statistical significance between the two groups (P< 0.001 for all). A stratified analysis of the two groups showed that the prevalence increased with age, and the prevalence among medical workers of all ages was higher than that of the health population younger than 50 years of age. Multivariate Logistic regression analysis showed that female sex (OR=1.646,95% CI: 1.315– 2.060), older age (OR=1.384,95% CI: 1.265– 1.514), and high BMI (OR = 1.199, 95% CI: 1.065– 1.350) were risk factors for the disease among medical staff. In the health population, female sex (OR=0.799,95% CI: 0.644– 0.992) and high TSH levels (OR = 0.918, 95% CI: 0.874– 0.964) were protective factors, while older age (OR=1.634,95% CI: 1.525– 1.751) was a risk factor.
Conclusion: There are certain differences in the prevalence of thyroid nodules between the two groups. Age and occupation are important influencing factors. While age is uncontrollable, active regulation of emotional status caused by occupational factors has important clinical guiding significance for reducing the prevalence of thyroid nodules and reducing the social medical burden.
Keywords: thyroid nodules, prevalence, risk factors, medical staff, healthcare professions, occupational health
Introduction
In one of the largest endocrine glands in the human body, the thyroid gland, which consists of two connected lobes, different thyroid lesions are often found, and the majority of these lesions are non-cancerous, so-called benign lesions, which include simple or hemorrhagic cysts, thyroid nodules, and thyroid adenomas.1 Thyroid nodules (TNs) are scattered lesions caused by abnormal hyperplasia of thyroid cells. They originate from thyroid follicular cells and usually have benign nature. Compared with other endocrine diseases, they lack specific symptoms and are often found to coexist with other thyroid pathologies. With the increasing usage of the Color Doppler ultrasound and other sophisticated imaging methods in medical examination, the detection rate of TNs reached 20%–76%, and the prevalence rate tends to increase with age.2,3 A significant portion of TNs is incidental findings – when imaging was done for other medical indications, and these are so-called “incidentalomas”. The main risk factors identified to date are female sex, iodine deficiency and head and neck irradiation.4–6 Although commonly benign, TNs deserve clinical attention and follow-up upon diagnosis, since approximately 5%–15% TNs can become malignant.7 Obviously, this is accompanied with a certain economic and living burden for the society, patients and their families. Upon diagnosis of TNs, it is of particular importance to follow-up patients with family history of thyroid carcinomas, childhood irradiation, and those with nodules that exhibit rapid growth.8 In addition to malignant potential of some TNs, they often may cause other clinical manifestations, such as thyroid dysfunction, compressive symptoms, hoarseness, dysphagia, shortness of breath, and pain.9,10 Patients with diagnosed TNs must be further managed by ultrasound and/or other imaging techniques, fine needle aspiration biopsies followed by cytology and often with molecular diagnostics,11–14 which is laborious, time-consuming and expensive.
Therefore, it is particularly important to carry out targeted early prevention and control of TNs to reduce the time for progression, as well as to characterize all related factors relevant for further monitoring. Völzke and co-workers found that TNs are related to high serum IGF-I (Insulin-Like Growth Factor-I) levels in men, and to decreased serum TSH (Thyroid Stimulating Hormone) levels in women.15 Two recently published epidemiological studies from China, comprehensively analyzed prevalence of TNs and report the regional specific pattern and correlation with iodine concentration in drinking water.16,17
Interestingly, although it has been hypothesized that the influence of emotional factors, mood disorders, and psychological stress might be connected with thyroid diseases, there are no studies regarding their correlation with TNs. Thyroid dysfunction has long been associated with alterations in mood and cognition; moreover, anxiety and depression are highly prevalent among thyroid disorder patients.18,19 One of the frequently mentioned non-genetic risk factors for thyroid diseases such as Graves’ disease and Hashimoto’s thyroiditis is psychological stress.20–23
Having in mind that some professions might significantly influence health, we performed the study in which we analyzed the prevalence of thyroid nodules among medical staff and health check-up population in primary-level hospital, in Jinan City, in Shandong Province, China. A primary hospital is a township hospital (community health center) that provides general and preventive healthcare, minimal health care and rehabilitation services. In this paper, we analyzed the medical examination data of medical staff and general healthy population going to a routine check-up, and preliminarily discuss the factors related to TNs within these two groups, so as to provide guidance for more efficient prevention and early clinical management.
Study Subjects and Methods
Study Subjects
A total of 5812 health examination reports from our hospital in 2021 were selected, including 3341 males and 2471 females, ranging in age from 21 to 98 years with an average of (48.98± 15.49) years. Among them, 2388 were medical workers, and 3.424 were health check-up group (which consisted mainly from administrative workers, police workers, lawyers and teachers).
For each participant, information including age, gender, location, body mass index (BMI), systolic blood pressure (SBP), blood glucose, high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), uric acid (UA), free triiodothyronine (FT3), free thyroxine (FT4) and thyroid stimulating hormone (TSH) was collected from medical records. The research has been reviewed and approved by the Medical Ethics Committee of the hospital. Clinical and pathohistological dataset is provided in supplementary material (Supplementary Table 1).
Research Methods
Diagnostic Criteria
The hospital’s physical examination center carried out the examination and report of all physical examination items in strict accordance with the corresponding medical standards: i) thyroid ultrasound examination was carried out according to the Guidelines for Diagnosis and Treatment of Thyroid Nodules and Differentiated Thyroid Cancer (2012 Edition);2 ii) Diabetes was diagnosed according to “Guidelines for Prevention and Treatment of Type 2 Diabetes in China (2020 Edition)”24 iii) The blood pressure grade was determined according to “Guidelines for Prevention and Treatment of Hypertension in China (2018 Edition)”25 iv) BMI was graded according to “China Adult Overweight and Obesity Prevention and Control Guidelines (2006 Edition)”26 All biochemical parameters were determined according the standard diagnostic procedures.
Inclusion Criteria
The inclusion criteria were as follow: 1. On-the-job medical staff and health check-up population in the hospital; 2. Ultrasonic report of thyroid gland is complete; 3. The three test indexes of A-power are intact.
Quality Control
All venous blood was collected on an empty stomach before 10:00 a.m. (fasting glucose level) and sent to the laboratory of this hospital for testing. Ultrasonic examination is performed independently by two ultrasonic specialists with more than 3 years clinical experience in this hospital, and it is strictly carried out in accordance with the corresponding professional standards. If there was any disagreement with the diagnosis conclusion, the third doctor would have been asked to review the diagnosis. Two researchers independently counted the relevant data included in the report and entered the data by double entry.
Processing of Missing Values
When the missing ratio of each observation index data is less than 20%, the regression estimation method is used to fill in.
Statistical Analysis
SPSS 25.0 was used for data statistical analysis. For measured data which were normally distributed, an independent sample t-test was used for comparison between groups. The data were expressed as percentage, and the comparison between groups was tested by chi-square (χ2) test. Multivariate Logistics regression analysis is used to determine whether there is a causal relationship between variables. P value less than 0.05 was considered statistically significant.
Results
Missing Value Filling
All the missing values are completely random, and the missing ratio is less than 20%. In the subgroup of medical staff, all gender and age data were available, but data deficiencies were detected for: BMI - 13.20%, SBP - 12.44%, blood glucose - 17.67%, HDL-C - 7.66%, LDL-C - 4.70% and uric acid (UA) - 2.85% (percentage of loss rate). In the subgroup of health population, there was no deficiency in data regarding the gender, age and fasting blood glucose, but data deficiencies were detected for: BMI - 9.23%, SBP - 6.89%, HDL-C - 0.23%, LDL-C - 0.09% and UA - 0.03%. The missing data of both groups were filled by regression estimation.
Prevalence of Thyroid Nodules in Examined Groups
A medical staff examined group consists of 2388 medical workers (median age 36.20 ± 9.11) in total, including 556 males (median age 35.59 ± 8.65) and 1832 females (median age 38.22 ± 10.23). In the health check-up group, there were 3424 subjects (median age of 57.89 ± 12.51), including 2785 males (median age 58.77 ± 12.00) and 639 female patients (median age 54.02 ± 13.88). The average age difference between the two groups was statistically significant (t = 72.384, P < 0.001), and the age differences between different sexes were statistically significant (all P < 0.001). In the whole cohort, the total prevalence was 57.6% (3347 TN positive cases out of 5812 subjects). The total prevalence rate of medical staff was 48.5%, with 41.9% in men and 50.5% in women subgroup, with a significant difference (χ2 = 12.586, P < 0.001); The total prevalence rate of health check-up group was 63.9%, of which 66.5% was male and 52.7% was female, and the difference was statistically significant (χ2 = 42.679, P < 0.001) (Table 1). According to the stratified analysis of different age groups, the prevalence rates of both groups showed an increasing trend with age. The prevalence rates of female medical staff in all age groups were higher than those of men, while the healthy population showed higher prevalence in men (except for the age group 50–60 years where the prevalence is similar). The prevalence rates of medical staff in all age groups up to the age of 50 were significantly higher than those of health check-up population, as shown in Figure 1.
 |
Table 1 Prevalence and Gender Differences of Thyroid Nodules (TNs) in Two Groups |
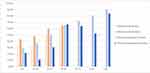 |
Figure 1 Prevalence of TNs in different ages and sexes in two groups. Notes: X axis – years, Y axis – percentage. |
Having in mind that there are other stressful professions, we analyzed subgroups of health check-up population (where data available) and found that the subgroup of police workers also had high prevalence of TN (473 out of 642, 73.7%), with significant difference (χ2 = 61,399, P < 0.001) compared to other professions (lawyers, teachers, administrative staff) (data not shown).
Differences of FT3, FT4 and TSH Levels
The levels of FT3, FT4 and TSH in subjects below 30 years old were analyzed, and there was no significant difference between medical staff and healthy population (P = 0.742, 0.124 and 0.815, respectively). However, there were significant differences in FT3 and TSH levels in all age groups over 30 (all P < 0.05). In addition, there were significant differences in FT4 levels between 30 and 50 years old (all P < 0.05), as shown in Table 2.
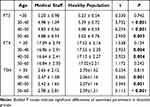 |
Table 2 Differences of FT3, FT4 and TSH Levels Between Groups and Ages (x s) |
Univariate Analysis of Risk Factors of TNs
Univariate analysis was made on 11 indexes of sex, age, BMI, SBP, diabetes, FT3, FT4, TSH, HDL-C, LDL-C and UA of the two examined groups. The results showed that there were significant differences in sex, age, BMI, FT3 and HDL-C between the medical staff with and without thyroid nodules (all P < 0.05), but not in systolic blood pressure and diabetes. There are statistically significant differences in sex, age, BMI, systolic blood pressure, FT3, TSH, HDL-C and UA between healthy people with and those without thyroid nodules (all P < 0.05), but there are no statistically significant differences in diabetes, FT4 and LDL-C (all P > 0.05) (Table 3).
 |
Table 3 Univariate Analysis of Related Factors of TNs in Two Groups |
Multivariate Logistic Regression Analysis
According to the results of univariate analysis of two groups, multivariate Logistic regression analysis was carried out with statistically significant indicators of each group as independent variables. The results showed that gender, age and BMI were the influencing factors for TNs positivity of medical staff, while gender, age, TSH and UA levels were the influencing factors for TNs positivity among the healthy population (Tables 4 and 5).
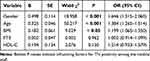 |
Table 4 Logistic Regression Analysis of Influencing Factors of TNs Among Medical Staff |
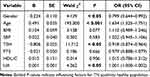 |
Table 5 Logistic Regression Analysis of Influencing Factors of TNs in Healthy Population |
Discussion
In recent years, with the change of social life, the number of patients with TNs has been increasing, with the average time of detection shifted towards younger age, which leads to a significant increase in the rate of unnecessary surgeries, at least in some percentage of patients.2 The potential risk of malignant transformation also brings great mental stress27 to a large number of patients with TNs, affecting their daily work and life. Therefore, it is of great significance to explore all related factors for TNs and guide clinical early prevention. This is especially important in the context of detection of those population groups that carry an increased risk for the formation of nodules: female sex, iodine deficiency and head and neck irradiation.3–5 Color Doppler ultrasound has the advantages of “non-invasive, painless, radiation-free, repeatable examination and simple operation”. It has high diagnostic sensitivity to TNs28 and can accurately evaluate the nature and morphological characteristics of nodules. Its sonogram can be associated with different lesions, and it has been recognized as the first choice for examination and evaluation of TNs.29
The results of sampling analysis of the medical examination report of a 3A hospital (Primary-level hospital) in Jinan show that the detection rate of TNs in the two groups is relatively high, but still in the range of reported prevalence in general population (5.2 to 67.0%).30 This finding is in accordance with the reported sensitivity of ultrasound and significance of timely examination for TN detection. In this study, the prevalence rates in both groups are increasing with age, and some detected differences are in concordance to the current research conclusions and results of others.31 Nowadays, it is generally accepted that, in addition to the above mentioned and confirmed risk factors, occupational stress, bad mood and anxiety are among the major risk factors for development of TNs.32–35 The average age of healthy population subgroup of our cohort was 57.89 ± 12.51 years, which was significantly higher than that of medical workers (36.20 ± 9.11 years) (t = 72.384, P < 0.001). The total prevalence rate in healthy population was 63.9%, which was also significantly higher than that of medical workers (48.5% (χ2 = 137)), and this finding is probably due to the older age in healthy population group. Interestingly, through stratified analysis of the two groups (from the same region), it is found that the prevalence rate among medical staff younger than 50 is significantly higher than that of healthy population. Although no relevant stress and psychological evaluation has been conducted in this study, we hypothesized that higher prevalence of TNs in medical staff younger than 50 years might be related to the specific occupational factors of medical staff. Their work pressure and mental stress are high, and obesity, often caused by lack of exercise, is quite prominent,36 which is consistent with the research conclusions of Wang Junming.37 In the study of Harbeck and coworkers, biochemical and physiological stress parameters were analyzed among young physicians (range 26–42 years) before and after 24- hour on-call shifts (OCS) in internal medicine.38 They found that the levels of thyroid stimulating hormone (TSH) were significantly higher after a 24- hour OCS, while there were no significant changes in cortisol, epinephrine, and norepinephrine levels. Their findings clearly indicate that disruption of circadian rhythm and sleep/wake cycles leads to increase in TSH levels, suggesting that TSH might serve as an early and sensitive biochemical predictor of stress. In another study, Afrashteh et al showed that stress and low-quality sleep were associated with the risk of thyroid cancer, while good-quality sleep had a protective effect.39 However, after the age of 50, the knowledge reserve and clinical experience of medical staff have reached a higher level, and their occupational pressure might have been relatively reduced, so the difference of prevalence between the two groups has narrowed. The prevalence rate of medical workers in all ages is higher in women than in men, while that of healthy population after age of 60 years is higher in men than in women. The finding that prevalence of TNs is higher among female medical workers may be addressed to different receptivity of women (more empathy to patients, etc.). It is also possible that women are more sensitive to disturbing the circadian rhythm due to the night shifts in hospital. Interestingly, we detected significantly higher prevalence of TNs in the subgroup of police workers (within the health-checkup group), and this finding might also be associated with overnight work shifts. The detected differences in three parameters related to thyroid (FT3, FT4 and TSH) between the two examined groups, after the age of 30, might be due to the different psychological and emotional capacity (probably as a consequence of the differences in educational level and occupation). Some studies have pointed out that the hypothalamus-pituitary-thyroid axis has a certain correlation with anxiety disorders, and this influence is related to TSH level.40 Thyroid hormones play an important role in the adult brain function and disturbance of thyroid metabolism in the brain may affect mental function, cognition and emotions.41–43 Despite the fact that the role of thyroid hormones in the adult brain is not fully resolved yet, it was showed that thyroid dysfunction may be connected with mood, cognition and some psychiatric symptoms. However, since peripheral thyroid function may not adequately reflect central thyroid metabolism and function, this is still an open issue.43 In the presented study, a multivariate logistic regression analysis showed that female sex, increasing age and high BMI were the major risk factors of the disease among medical staff. On the contrary, among healthy population female sex is protective factor, as well as higher TSH and UA levels, while advanced age is a risk factor. Although our study shows that TSH levels in the medical staff group are not associated with TNs, we detected higher TSH levels in this group compared to health-checkup group (in all age groups above 30 years), which is in line with the findings of Harbeck and coworkers.38
According to this study, the prevalence rate in the whole cohort examined, as well as in the analyzed subgroups is somewhat higher than values reported for Shandong province in two recently published epidemiological studies.16,17 Shandong is already among the provinces with highest prevalence of TNs in China, and higher values in our study might be due to some specificity of Jinan area, as well as due to the structure of the examined cohort. Furthermore, some uncontrollable environmental factors (such as pollution, pesticide residues, with endocrine disrupting activity) might cause higher prevalence of TNs.44
Taken together, the results of this study suggest that gender, age and occupation are the major influencing factors of TNs, with gender and age being uncontrollable. Therefore, our results indicate that more attention should be paid to the influence of occupational factors on TNs and further epidemiological research should be conducted with the aim to identify professions with higher risk. Leaders of relevant units can regularly organize mental health education and adjust their working methods, as well as working time appropriately and reasonably, so as to reduce the occurrence of TNs among their employees and reduce the social medical burden. On the other hand, thyroid nodules are commonly benign, and ultrasonography can detect nodules that are rather small and have undetermined clinical significance.45 The new imaging methods for predicting malignant potential of TNs, like elastography and 18F-fluorodeoxyglucose positron emission tomography (18FDG-PET) are developed, but ultrasound is still one of the main tools for determining the risk of cancer in a given nodule.45
Having in mind that incidental malignancy was found in 1.53% (8/522) of thyroid nodules classified as Bethesda II category,46 and between 15 and 40% of thyroid nodules that fall within Bethesda categories III–IV,47 it is clear that histopathology finding is also necessary for further decision about treatment options. According to Mulita and coworkers,48 the patients with atypia of undetermined significance [AUS] or follicular lesion of undetermined significance [FUS] (Bethesda category III) may have a higher risk of malignancy than traditionally believed. Therefore, an appropriate surgical treatment48,49 might be an option, at least in the certain subgroups of TNs positive cases, that fall at higher risk, according to histopathology.
Since this study is a cross-sectional study, the relationship between research factors and conclusions is exploratory; its exact causal relationship needs to be further confirmed by a future prospective and studies. In addition, because this study has some shortcomings in the sample number and sample selection, a more extensive epidemiological investigation with a carefully designed cohort will be necessary for a more reliable exploration of the risk factors for TNs, especially directed towards detection of potential relation to various occupational factors.
Conclusion
In this study, we confirmed that in addition to gender and age, professions related to night shifts might be considered as potential risk factors for thyroid nodules. Therefore, more attention should be paid to the influence of occupational factors on TNs in order to identify professions with higher risk. Regardless of the fact that TNs are usually benign lesions, a certain percentage can evolve into malignant entities, and therefore identification of additional risk factors is extremely important in order to reduce their occurrence and the accompanying social medical burden.
Data Sharing Statement
The data for this research are available in the supplementary dataset, where all data have been de-identified and there is no potential to breach patient confidentiality by including Physical Examination ID numbers.
Ethics Statement
The studies involving humans were approved by the Ethics Committee of Central Hospital Affiliated to Shandong First Medical University (2021-ZXYY-127). The studies were conducted in accordance with the Declaration of Helsinki, and the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Funding
There is no funding to report.
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Mulita F, Anjum F. Thyroid adenoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 32965923.
2. Endocrinology Branch of Chinese Medical Association. Guidelines for diagnosis and treatment of thyroid nodules and differentiated thyroid cancer. Chin J Endocrinol Metab. 2012;28(10):779–797.
3. Durante C, Grani G, Lamartina L, et al. The diagnosis and management of thyroid nodules: a review. JAMA. 2018;319(9):914–924. doi:10.1001/jama.2018.0898
4. Gharib H. Changing concepts in the diagnosis and management of thyroid nodules. Endocrinol Metab Clinics North Am. 1997;26(4):777–800. doi:10.1016/S0889-8529(05)70282-6
5. Leech JV, Smith LW, Clute HM. Aberrant thyroid glands. Am J Pathol. 1928;4(5):481–492.
6. Rojeski MT, Gharib H. Nodular thyroid disease: evaluation and management. New Engl J Med. 1985;313(7):428–436. doi:10.1056/NEJM198508153130707
7. Touzopoulos P, Karanikas M, Zarogoulidis P, et al. Current surgical status of thyroid diseases. J Multidiscip Healthc. 2011;4:441–449. doi:10.2147/JMDH.S26349
8. Wong R, Farrell SG, Grossmann M. Thyroid nodules: diagnosis and management. Med J Aust. 2018;209(2):92–98. doi:10.5694/mja17.01204
9. Popoveniuc G, Jonklaas J. Thyroid nodules. Med Clin N Am. 2012;96(2):329–349. doi:10.1016/j.mcna.2012.02.002
10. Knox MA. Thyroid nodules. Am Fam Physician. 2013;88(3):193–196.
11. Holt EH. Current Evaluation of Thyroid Nodules. Med Clin North Am. 2021;105(6):1017–1031. PMID: 34688412. doi:10.1016/j.mcna.2021.06.006
12. Alexander EK, Doherty GM, Barletta JA. Management of thyroid nodules. Lancet Diabetes Endocrinol. 2022;10(7):540–548. PMID: 35752201. doi:10.1016/S2213-8587(22)00139-5
13. Kobaly K, Kim CS, Mandel SJ. Contemporary management of thyroid nodules. Annu Rev Med. 2022;73(1):517–528. PMID: 34416120. doi:10.1146/annurev-med-042220-015032
14. Alexander EK, Cibas ES. Diagnosis of thyroid nodules. Lancet Diabetes Endocrinol. 2022;10(7):533–539. PMID: 35752200. doi:10.1016/S2213-8587(22)00101-2
15. Völzke H, Friedrich N, Schipf S, et al. Association between serum insulin-like growth factor-I levels and thyroid disorders in a population-based study. J Clin Endocrinol Metab. 2007;92(10):4039–4045. PMID: 17666480. doi:10.1210/jc.2007-0816
16. Li Y, Jin C, Li J, et al. Prevalence of thyroid nodules in china: a health examination cohort-based study. Front Endocrinol. 2021;12:676144. doi:10.3389/fendo.2021.676144
17. Yu Z, Mingkun T, Yingying W, et al. Prevalence of thyroid nodules and its association with water iodine among Chinese men and women. Environ Res. 2022;212:113270. doi:10.1016/j.envres.2022.113270
18. Ritchie M, Yeap BB. Thyroid hormone: influences on mood and cognition in adults. Maturitas. 2015;81(2):266–275. PMID: 25896972. doi:10.1016/j.maturitas.2015.03.016
19. Gorkhali B, Sharma S, Amatya M, Acharya D, Sharma M. Anxiety and Depression among Patients with Thyroid Function Disorders. J Nepal Health Res Counc. 2020;18(3):373–378. PMID: 33210626. doi:10.33314/jnhrc.v18i3.2499
20. Fukao A, Takamatsu J, Arishima T, et al. Graves’ disease and mental disorders. J Clin Transl Endocrinol. 2019;19:100207. PMID: 31763175; PMCID: PMC6864135. doi:10.1016/j.jcte.2019.100207
21. Ajjan RA, Weetman AP. The pathogenesis of hashimoto’s thyroiditis: further developments in our understanding. Horm Metab Res. 2015;47(10):702–710. PMID: 26361257. doi:10.1055/s-0035-1548832
22. Mikoś H, Mikoś M, Obara-Moszyńska M, Niedziela M. The role of the immune system and cytokines involved in the pathogenesis of autoimmune thyroid disease (AITD). Endokrynol Pol. 2014;65(2):150–155. PMID: 24802739. doi:10.5603/EP.2014.0021
23. Marinò M, Latrofa F, Menconi F, et al. Role of genetic and non-genetic factors in the etiology of Graves’ disease. J Endocrinol Invest. 2015;38(3):283–294. doi:10.1007/s40618-014-0214-2
24. Diabetes Branch of Chinese Medical Association. Guidelines for Prevention and Treatment of Type 2 Diabetes in China (2020) [J]. Int J Endocrinol Metab. 2021;41(05):482–548.
25. Liu L, Wu Y, Wang J, Wang W. China guidelines for prevention and treatment of hypertension revised in 2018. Prev Treat Cardiovasc Cerebrovasc Dis. 2019;19(01):1–44.
26. Leong W-I, Lönnerdal B; China Obesity Working Group. Guidelines for prevention and control of overweight and obesity among adults in China (excerpt). J Nutr. 2004;134(1):1–4. doi:10.1093/jn/134.1.1
27. Jiang J. Study on psychological status and quality of life of patients with thyroid nodules [Dissertation]. Shandong University; 2017.
28. Song J, Liu Y, Zeng X, et al. Comparative study of color Doppler ultrasound combined with tissue elastography in the diagnosis of thyroid nodules. Chin J Ultrasound Med. 2015;31(08):673–675.
29. Lingling T, Wang T, Shen Y, et al. Preliminary study on morphological characteristics of thyroid nodules by contrast-enhanced ultrasound. China J Med Comput Imaging. 2015;21(01):73–76.
30. Karaszewski B, Wilkowski M, Tomasiuk T, et al. Czestość wystepowania guzków incydentalnych w tarczycy w populacji mieszkańców Trójmiasta (Gdańsk, Sopot, Gdynia) [The prevalence of incidentaloma--asymptomatic thyroid nodules in the Tricity (Gdansk, Sopot, Gdynia) population]. Endokrynol Pol. 2006;57(3):196–200. Polish. PMID: 16832782.
31. Xu H, Cui Y, Lan M, et al. Investigation of thyroid nodules in healthy people and analysis of influencing factors. Chin Gene Prac. 2014;12(05):784–785.
32. Yahui T, Feifei B, Geling L. Analysis of thyroid nodules and related risk factors in Tangshan [J]. Occup Healt. 2014;30(23):3415–3417.
33. Lang F, Wang W, Zheng D, et al. Study on the correlation between thyroid nodules and anxiety and depression among teachers in a university in Weifang [J]. J Weifang Med Coll. 2019;41(04):259–262.
34. Jie H, Xia Y, Xue J, et al. Prevalence and influencing factors of thyroid nodules in Zhengzhou community residents. China Public Health. 2014;30(08):1022–1025.
35. Wang Q, Chen Y. Analysis of the prevalence of thyroid nodules and related risk factors among healthy people. China Med Front J. 2017;9(10):183–187.
36. Guo L, Ma Z, Hao Y. Analysis of body fat composition and health status of medical staff in a tertiary hospital in Beijing. Hebei Med. 2021;43(06):937–940.
37. Wang J, Hao Z, Chen C, et al. Study on the detection rate and characteristics of thyroid nodules in different occupational groups in Shijiazhuang. China Gene Med. 2012;15(36):4193–4195+4199.
38. Harbeck B, Suefke S, Haas CS, Lehnert H, Kropp P, Moenig H. No stress after 24-hour on-call shifts? J Occup Health. 2015;57(5):438–447. PMID: 26119209; PMCID: PMC6706192. doi:10.1539/joh.14-0276-OA
39. Afrashteh S, Fararouei M, Parad MT, Mirahmadizadeh A. Sleep quality, stress and thyroid cancer: a case-control study. J Endocrinol Invest. 2022;45(6):1219–1226. PMID: 35112324. doi:10.1007/s40618-022-01751-4
40. Fischer S, Ehlert U. Hypothalamic-pituitary-thyroid (HPT) axis functioning in anxiety disorders. A systematic review. Depress Anxiety. 2018;35(1):98–110. doi:10.1002/da.22692
41. Li L, Zhi M, Hou Z, et al. Abnormal brain functional connectivity leads to impaired mood and cognition in hyperthyroidism: a resting-state functional MRI study. Oncotarget. 2017;8(4):6283–6294. doi:10.18632/oncotarget.14060
42. Schroeder AC, Privalsky ML. Thyroid hormones, t3 and t4, in the brain. Front Endocrinol. 2014;5:40. doi:10.3389/fendo.2014.00040
43. Bauer M, Goetz T, Glenn T, Whybrow PC. The thyroid-brain interaction in thyroid disorders and mood disorders. J Neuroendocrinol. 2008;20(10):1101–1114. doi:10.1111/j.1365-2826.2008.01774.x
44. Leemans M, Couderq S, Demeneix B, Fini JB. Pesticides with potential thyroid hormone-disrupting effects: a review of recent data. Front Endocrinol. 2019;10:743. PMID: 31920955; PMCID: PMC6915086. doi:10.3389/fendo.2019.00743
45. Dean DS, Gharib H. Epidemiology of thyroid nodules, best practice. Res Clin Endocrinol Metab. 2008;22(6):901–911. ISSN 1521-690X. doi:10.1016/j.beem.2008.09.019
46. Mulita F, Iliopoulos F, Tsilivigkos C, et al. Cancer rate of Bethesda category II thyroid nodules. Med Glas. 2022;19(1). PMID: 34734516. doi:10.17392/1413-21
47. Mulita F, Plachouri MK, Liolis E, Vailas M, Panagopoulos K, Maroulis I. Patient outcomes following surgical management of thyroid nodules classified as Bethesda category III (AUS/FLUS). Endokrynol Pol. 2021;72(2):143–144. PMID: 33749812. doi:10.5603/EP.a2021.0018
48. Mulita F, Verras GI, Dafnomili VD, et al. Thyroidectomy for the management of differentiated thyroid carcinoma and their outcome on early postoperative complications: a 6-year single-centre retrospective study. Chirurgia. 2022;117(5):556–562. PMID: 36318685. doi:10.21614/chirurgia.2736
49. Mulita F, Theofanis G, Verras GI, et al. Comparison of postoperative bleeding using harmonic scalpel and LigaSure in thyroid surgery: a 15-year single-centre retrospective study. Med Glas. 2023;20(2). PMID: 37585298. doi:10.17392/1629-23
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Psychological Impact of Quarantine During the COVID-19 Pandemic on Quarantined Non-Healthcare Workers, Quarantined Healthcare Workers, and Medical Staff at the Quarantine Facility in Saudi Arabia
Alfaifi A, Darraj A, El-Setouhy M
Psychology Research and Behavior Management 2022, 15:1259-1270
Published Date: 17 May 2022
Anaemia, Morphological Classification and Its Associated Risk Factors Among Lactating Mothers at Mbarara City Council Health Centre IV, Southwestern Uganda
Clinton O, Micheal K, Namyalo Angella K, Mary M, Mike M, Muwanguzi E, Okongo B, Wagubi R
Journal of Blood Medicine 2022, 13:473-481
Published Date: 2 September 2022
Dry Season Eimeria Infection in Dairy Cattle and Sheep in and Around Adama and Bishoftu Towns, Oromia, Ethiopia
Ayana D, Temesgen K, Kumsa B, Alkadir G
Veterinary Medicine: Research and Reports 2022, 13:235-245
Published Date: 9 September 2022
Chronic Obstructive Pulmonary Disease Prevalence and Associated Risk Factors in Adults Aged 40 Years and Older in Southeast China: A Cross-Sectional Study During 2019–2020
Chen J, Yin Y, Zhang Y, Lin X, Chen T, Yang Z, Wang D, Zhong W
International Journal of Chronic Obstructive Pulmonary Disease 2022, 17:2317-2328
Published Date: 17 September 2022
Prevalence, Management, and Risk Factors of Asthma Among School-Age Children in Yogyakarta, Indonesia
Triasih R, Setyowireni D, Nurani N, Setyati A
Journal of Asthma and Allergy 2023, 16:23-32
Published Date: 5 January 2023
