Back to Journals » Clinical Optometry » Volume 16
Public Awareness, Knowledge of Presbyopia and Compliance to Eye Examination in Jordan
Authors Haddad MF, Abdo N, Bakkar MM
Received 8 March 2024
Accepted for publication 18 July 2024
Published 29 July 2024 Volume 2024:16 Pages 191—199
DOI https://doi.org/10.2147/OPTO.S467933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Mera F Haddad,1 Nour Abdo,2 May M Bakkar1
1Department of Allied Medical Sciences, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Public Health, Jordan University of Science and Technology, Irbid, Jordan
Correspondence: Mera F Haddad, Department of Allied Medical Sciences, Jordan University of Science and Technology, POBox 3030, Irbid, 22110, Jordan, Tel +962797151304, Email [email protected]
Purpose: To assess public awareness and knowledge about presbyopia and their compliance to ocular examination in Jordan.
Patients and Methods: A cross-sectional survey was designed to interview people in different provinces of Jordan. Socio-demographic data such as age, gender and level of education and region was reported. The first part of the questionnaire assessed awareness of presbyopia in terms of the need for spectacles with age, age of onset, possible causes of presbyopia and methods of presbyopia management. The second part of the questionnaire evaluated compliance of the participants with ocular examination in terms of frequency and motive to do general eye check, intraocular pressure (IOP), fundus exam and visual acuity.
Results: A total of 802 participants (232 males, 570 females) with an average age of 28 (± 11.6) completed the questionnaire. Most participants (84.2%) knew that glasses are needed for near vision as age increases, and 62.8% estimated the age at which spectacles are required (40 years or older). Over half understood that presbyopia is correctable and progressive. Age significantly influenced knowledge about the need for near vision spectacles, and whether presbyopia is preventable and progressive (both p < 0.05). Females were more knowledgeable about these aspects. The frequency of eye examinations, particularly fundus exams and IOP tests, was significantly influenced by age but not by education. Gender only significantly affected the frequency of vision checks (p = 0.01), with females being more likely to adhere to them.
Conclusion: This study demonstrated a good level of awareness and knowledge about presbyopia among Jordanians, especially those over 40 and females. Regular eye check-ups were more common among young participants and females. Addressing misconceptions about presbyopia’s preventability and promoting regular eye exams are crucial for early diagnosis and management of presbyopia and other serious eye conditions.
Keywords: awareness, presbyopia, eye examination, Jordan
Introduction
Presbyopia is an age-related vision condition, and if uncorrected, it is considered the most common cause of visual impairment at near.1,2 The most common cause of presbyopia is the natural ageing process of the lens inside the eye, which involves reduction in the elasticity of the lens fibers, thus reducing its ability to accommodate to focus near objects. The major risk factor for presbyopia is increasing age, although other factors have been reported such as disease, trauma and medication.3 Currently, presbyopia can be corrected optically using glasses (single vision, bifocal and progressive lenses) or contact lenses (bifocal, multifocal) and surgically using accommodative intra-ocular lenses at the time of cataract surgery or laser or conventional corrective surgical techniques.4,5
Many reports have been published about the prevalence of presbyopia in countries around the world. According to the World Health Organization, the global prevalence of presbyopia is high reaching to 1.8 billion (including both addressed and unaddressed).6 Most studies have shown a high prevalence of presbyopia with a reduced met need for presbyopia correction, ie spectacle coverage was very low among presbyopic patients.7–9 For example, in rural northern China, the prevalence of presbyopia was very high (69%), and nearly half of the affected persons were not corrected.10 In Kenya, a country with low income, the prevalence was even higher around 80%, and 62% of them were not corrected.11 According to Bourne et al, there are 1097.4 million people globally who had visual impairment as a result of uncorrected presbyopia.1
The barriers to not seeking medical care for the correction of presbyopia have also been discussed extensively. In areas with low income, the cost of glasses or other methods of correction was the main barrier for not meeting their vision correction needs.11,12 The lack of awareness about the condition, the lack of felt need for correction, and poor quality of available glasses were also described as barriers for not obtaining spectacle correction.7,10 Access to services for testing the vision was also reported by the African population.13
In addition to the impact of presbyopia on the quality of vision, presbyopia can significantly influence the quality of life of presbyopes. This finding has been reported both for developed and developing countries. Bekibele & Gureje14 found that reduced vision at near affected all domains of quality of life, ie physical, psychological and social aspects of daily life. This was confirmed by Lu et al15 who reported that presbyopes were ashamed and embarrassed due to their vision problems and thus had diminished practice of household activities, social interactions, work and leisure-time pursuits compared to non presbyopes. Correction of presbyopic vision and stereoacuity, on the other hand, significantly improved the quality of life of presbyopes16 and increased productivity of presbyopes at their workplace.17
It is obvious that the awareness of presbyopia and the need for regular eye examination are lacking. Therefore, we sought in this work to assess the awareness and knowledge of presbyopia in terms of etiology and correction and to evaluate participants’ compliance with ocular examination for vision check and other vision-related problems.
Materials and Methods
Study Design and Participants
A cross-sectional study was conducted using a semi-structured questionnaire developed in the Arabic language. Participants were asked to answer questions related to their awareness and knowledge about presbyopia. Participants were selected using cluster sampling targeting the north, middle and south of Jordan. Each region contains four governorates of which two were chosen randomly for the survey. The two governorates chosen included rural and urban districts. Participants aged ≥18 years old were approached to participate, and informed consent was obtained from all participants prior to their participation in the study.
The questionnaire was assessed by different faculty members in the Optometry department at Jordan University of Science and Technology. The questionnaire was reviewed by a senior epidemiologist and senior optometrist who agreed that the tool covers appropriate and adequate items to assess awareness and knowledge of presbyopia and adherence to ocular examination. The questionnaire was further reviewed by expert panel (including senior optometrists) and then distributed for testing by a pilot group (n = 30) to further assess clarity and relevance of survey questions. Pilot sample was conveniently chosen from one governorate in the north of Jordan from urban and rural districts. Comments and feedback by the pilot group was taken into consideration before the final survey was distributed to target population. Data from pilot group was not included in the final analysis.
Data Collection
The questionnaire was administered, by a trained optometrist, to willing participants and a face-to-face interview was conducted. The study lasted for 8 months, with data collection conducted from October 2022 to June 2023.
Data on socio-demographics such as age, gender, and level of education were collected. The participants were then asked to complete the questionnaire which assessed their knowledge about presbyopia. ‘Yes’ or “No” questions were asked about awareness of the need for glasses with age, if the condition was preventable, correctable, and progressive with age. Open-ended questions such as deciding the age at which presbyopia occurs, explanation of how it occurs, and knowledge of how it is corrected were also included.
The second part of the questionnaire assessed the compliance of participants with ocular examination and follow-up visits. Questions about the frequency of checking their ocular health in general, their intraocular pressure, retina and visual acuity were asked. These tests were specified as follows: Eye check or general eye exam: assessed the general health of the ocular surface, primarily the anterior segment (including the lid, lashes, cornea, and lens). IOP and fundus exam: focused mainly on the posterior segment. VA check: specifically measured visual acuity, primarily for the purpose of refraction and prescribing glasses.
Data Analysis
All data analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA). Descriptive frequencies and percentages were used to summarize categorical data. Bivariate comparisons between awareness of presbyopia and age were done using chi-square test for the categorical variables (gender and level of education). Fisher’s exact test was used for low counts. The level of significance was set at (p < 0.05).
Ethics Approval
Ethics approval for conducting the study was granted by the Institutional Review Board (IRB) at Jordan University of Science and Technology (JUST). An informed consent was obtained from all participants prior to their participation in the study, and the study protocol complied with the guidelines of the Declaration of Helsinki.18 To maintain confidentiality, participant identities were anonymized using codes for identification. Furthermore, stringent measures were implemented to secure the data, restricting access solely to the researchers directly participating in the study.
Results
Socio-Demographics of Participants
A total of 802 participants (232 males and 570 females) completed the questionnaire. The average age (± standard deviation) of participants was 28 ± 12 and it ranged from 18 to 80 years old. Table 1 shows the demographic distribution of the study participants.
 |
Table 1 Demographic Distribution of the Study Participants (n = 802) |
Awareness of Presbyopia
Table 2 shows the level of awareness of presbyopia among the participants. Most people 675 (84.2%) knew that glasses are required to correct vision at near with increased age and 504 (62.8%) estimated the age at which near vision spectacles are required to be ≥40 years old. However, more than half of the study participants 498 (62%) could not explain why presbyopia occurs. When people were asked about the correction of presbyopia, 587 participants (73.2%) reported that presbyopia is correctable, with glasses and/or contact lenses being the most commonly cited methods of correction. A high percentage 691 (86.2%) reported that presbyopia is a progressive condition and it increases with age.
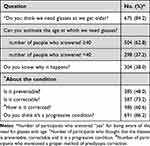 |
Table 2 Responses of Participants to Questions Related to Presbyopia (n = 802) |
Association Between the Level of Awareness of Presbyopia with Study Variables
The association between the level of awareness of presbyopia with study variables (age, gender and education) was also studied (Table 3). The results showed that the age of participants significantly influenced some of the responses related to presbyopia such as requiring near vision spectacles with age (p = 0.04), if the disease is preventable (p = 0.01) and progressive (p = 0.04). In addition, females were significantly more knowledgeable that glasses are required with age (p = 0.02) and that presbyopia is a preventable (p = 0.003) and progressive (p = 0.002).
 |
Table 3 Association of Awareness of Presbyopia with Subject Demography (Age, Gender and Education) (N = 802) |
Adherence to Ocular Examination
Figure 1 shows the frequency of eye examination in terms of general eye exam, IOP, retina and vision check as reported by the participants. The graph shows that 603 (75.2%) and 569 (71%) of the participants never tested their IOP and retina, respectively. On the other hand, a few people reported that they do these tests once a year (8.5%) or when they have problems or complaints (12%). The frequency of eye examination (general exam and refraction) was higher than those for IOP and retina tests. Most people (35%) reported that they test their eyes at least once a year. Many people reported that they check their eyes only when they have problems and that was reported more for vision and general eye exams (19.5%).
 |
Figure 1 Frequency of ocular examination as reported by participants (%). |
The association of the frequency of ocular examination with study variables (age, gender and education) was also tested (Table 4). The results show that the frequency of fundus exam and IOP test was significantly influenced by the age of the participant (both p < 0.05). The gender of participants, on the other hand, did not significantly affect the frequency of ocular examination apart from the vision check (p = 0.01) in which females appeared to adhere more to do vision check compared to males. The level of education did not significantly affect the frequency of ocular examination in all aspects.
 |
Table 4 Association of Different Eye Tests with Age, Gender and Education (n = 802) |
Discussion
Presbyopia is the most prevalent cause of vision impairment at near among people older than 40 years of age, and it is assumed to have zero prevalence in people younger than 30 years of age. The near visual impairment as a result of uncorrected presbyopia may result in visual stress and productivity loss that may affect the quality of life for people who perform near visual task such as reading and using computers and digital devices.2
The current study aimed to assess public awareness and knowledge about presbyopia among the population of Jordan. Many studies have distinguished between “awareness“ and “knowledge” of the disease. Awareness or familiarity with the disease requires the subject to have heard of the disease, whereas ”knowledge” requires better understanding of the disease and its aspects.19
The data showed that levels of both knowledge and awareness about presbyopia and its characteristics were high among the study participants. Most people knew about the need for spectacles with age and management options of presbyopia such as spectacles and contact lenses. Furthermore, most people who knew about contact lens options for the management of presbyopia reported the type of lenses used, ie, bifocal and multifocal. The relatively high level of awareness may be attributed to the powerful education system and feasible access to health-care services which are accessed by 95% of the population.
The level of awareness and knowledge about presbyopia was significantly affected by the age and gender of the participants. Individuals aged 40 and above were more knowledgeable about the necessity for spectacles with aging and understood that presbyopia is a progressive but correctable condition. This is not surprising, as presbyopia is age-related, and many participants in this age group may have already experienced its symptoms.
Females appeared to be significantly more aware about the need for spectacles with age and the progressive nature of the condition. This could be related to the near tasks practiced commonly by females and rarely done by males such as using makeup, sewing, cooking and other household chores that require good near vision. This could also be attributed to the retirement age of females at 55 years old20 which allows women more time to focus on their health, leading to more frequent visits to healthcare providers for regular eye check-ups, thus addressing age-related conditions like presbyopia. Additionally, retired women have more time to educate themselves about health issues, including presbyopia, increasing their awareness of the condition. For most Jordanian women, retirement also provides more opportunities to socialize and discuss common topics, including health issues.
Around 48% of the participants assumed that presbyopia is a preventable condition, although presbyopia occurs due to natural ageing of the eye’s lens and muscles and cannot be prevented. This high percentage could be related to misconceptions and beliefs in general health practice. There is a common believe that many age-related conditions are avoidable by healthy life style including exercise and healthy diet and this is applicable to presbyopia since it is an age-related condition. In addition, managing the symptoms of presbyopia such as reducing eye-strain or being a myope which may delay the occurrence may give the impression that presbyopia is a preventable eye condition.
The surprising finding is that people with higher levels of education reported that presbyopia is a preventable condition. This could be attributed to several factors related to the higher education levels of the participants. Firstly, highly educated individuals frequently use social media to seek information and integrate it into their education.21 Companies marketing eye care products and supplements on these platforms often emphasize the prevention of eye diseases, leading to the belief that presbyopia can be prevented. Secondly, educated people are more likely to be aware of advances in technology and treatments for eye diseases, such as LASIK and multifocal contact lenses, which may give the impression that presbyopia, like other age-related conditions, can be prevented or managed before its occurrence.
Adherence to Ocular Examination
Regarding adherence to ocular examinations, most participants did not regularly test their eyes for IOP or retinal health. However, a reasonable number of participants did have their eyes checked at least once a year. This is a positive finding, as regular eye check-ups are crucial for the early diagnosis of blinding conditions like glaucoma, macular degeneration, and other serious eye diseases. Consequently, patients visit eye clinics for general check-ups rather than specific tests like IOP measurements or fundoscopy.
This work has shown that young participants (ages 20–30) have a higher frequency of eye check-ups compared to other age groups. This age range includes university students and recent graduates who have just entered the workforce. University students often have access to free eye exams at on-campus optometry clinics, allowing them to undergo tests as frequently as needed. Recent graduates are typically required by their employers to have regular eye check-ups when they start working. These factors likely contribute to the higher frequency of eye examinations within this age group.
Females appeared to do regular vision check more than males. In general, research suggests that women are more health-conscious and seek medical help earlier than men do.22 This could be the case for eye health, leading to more regular eye examinations. Another reason could be that ocular changes, such as dry eye or other conditions due to hormonal fluctuations or household work, are more noticeable in women. This often prompts them to seek regular eye check-ups.23 On the other hand, males appeared to check their eyes only when necessary. This could be due to cultural norms which project a tough image about men and also men consider themselves less vulnerable to health issues. This may cause them to underestimate the need for regular check-ups including regular eye exam.
The current study has several limitations. Firstly, it aimed to study public awareness of presbyopia among different age groups. It would be more significant to assess awareness of the condition among affected people (presbyopes) at ages 40 years old and above. The second limitation is that the participants were not asked about possible ocular disease that could occur during presbyopic age. It is assumed that positive answer to this question may reflect better understanding of presbyopia and associated comorbidity in older population. Thirdly, the study could have recall and responder bias, particularly concerning the reported frequency of eye examinations. The fourth limitation is that the sample from the south was not representative and low number of participants was collected due to the difficulty in reaching cities in the south.
Conclusion
Near visual impairment due to presbyopia has a major influence on individual’s quality of life for people engaged in near visual tasks such as reading and using digital devices, etc. The awareness of presbyopia and the need for regular eye examination play an important role in reduced comorbidity related to the condition.
This study showed good level of awareness and knowledge about presbyopia among Jordanians, particularly among those above 40 and females, likely due to personal experience and engagement in near task. In terms of regular eye check-ups, they were more common among young participants and female, possibly due to accessibility to vision test and health consciousness, respectively.
Overall, addressing misconceptions about presbyopia in terms of preventability and promoting regular eye examinations are crucial for the early diagnosis and management of presbyopia and other serious eye conditions.
Acknowledgments
The authors would like to thank the deanship of research at Jordan University of Science and Technology for funding this work (grant#124) and all participants who took part in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bourne RRA, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888–e897. doi:10.1016/s2214-109x(17)30293-0
2. Fricke TR, Tahhan N, Resnikoff S, et al. Global prevalence of presbyopia and vision impairment from uncorrected presbyopia: systematic review, meta-analysis, and modelling. Ophthalmology. 2018;125(10):1492–1499. doi:10.1016/j.ophtha.2018.04.013
3. Mayo, clinic. Presbyopia. Available from: https://www.mayoclinic.org/diseases-conditions/presbyopia/symptoms-causes/syc20363328#:~:text=Presbyopia%20is%20caused%20by%20a,images%20appear%20out%20of%20focus.
4. Goertz AD, Stewart WC, Burns WR, Stewart JA, Nelson LA. Review of the impact of presbyopia on quality of life in the developing and developed world. Acta Ophthalmol. 2014;92(6):497–500. doi:10.1111/aos.12308
5. Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–143. doi:10.1016/j.preteyeres.2018.09.004
6. World report on vision; Licence: CC BY-NC-SA 3.0 IGO. World Health Organization; 2019.
7. Umar MM, Muhammad N, Alhassan MB. Prevalence of presbyopia and spectacle correction coverage in a rural population of North West Nigeria. Clin Ophthalmol. 2015;9:1195–1201. doi:10.2147/OPTH.S81194opth-9-1195
8. Mashayo ER, Chan VF, Ramson P, Chinanayi F, Naidoo KS. Prevalence of refractive error, presbyopia and spectacle coverage in Kahama District, Tanzania: a rapid assessment of refractive error. Clin Exp Optom. 2015;98(1):58–64. doi:10.1111/cxo.12207
9. Malhotra S, Vashist P, Kalaivani M, et al. Prevalence of presbyopia, spectacles coverage and barriers for unmet need among adult population of rural Jhajjar, Haryana. J Family Med Prim Care. 2022;11(1):287–293. doi:10.4103/jfmpc.jfmpc_1148_21JFMPC-11-287
10. Lu Q, He W, Murthy GVS, et al. Presbyopia and near-vision impairment in rural northern China. Invest Ophthalmol Visual Sci. 2011;52(5):2300–2305. doi:10.1167/iovs.10-6569
11. Sherwin JC, Keeffe JE, Kuper H, Islam FMA, Muller A, Mathenge W. Functional presbyopia in a rural Kenyan population: the unmet presbyopic need. Clin Exp Ophthalmol. 2008;36(3):245–251. doi:10.1111/j.1442-9071.2008.01711.x
12. Wubben TJ, Guerrero CM, Salum M, Wolfe GS, Giovannelli GP, Ramsey DJ. Presbyopia: a pilot investigation of the barriers and benefits of near visual acuity correction among a rural Filipino population. BMC Ophthalmol. 2014;14(1):9. doi:10.1186/1471-2415-14-9
13. Laviers HR, Omar F, Jecha H, Kassim G, Gilbert C. Presbyopic spectacle coverage, willingness to pay for near correction, and the impact of correcting uncorrected presbyopia in adults in Zanzibar, East Africa. Invest Ophthalmol Vis Sci. 2010;51(2):1234–1241. doi:10.1167/iovs.08-3154
14. Bekibele CO, Gureje O. Impact of self-reported visual impairment on quality of life in the Ibadan study of ageing. Br j Ophthalmol. 2008;92(5):612–615. doi:10.1136/bjo.2007.124859
15. Lu Q, Congdon N, He X, Murthy GV, Yang A, He W. Quality of life and near vision impairment due to functional presbyopia among rural Chinese adults. Invest Ophthalmol Vis Sci. 2011;52(7):4118–4123. doi:10.1167/iovs.10-6353
16. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optometry Vision Sci. 2006;83(5):266–273. doi:10.1097/01.opx.0000216098.62165.34
17. Reddy PA, Congdon N, MacKenzie G, et al. Effect of providing near glasses on productivity among rural Indian tea workers with presbyopia (PROSPER): a randomised trial. Lancet Glob Health. 2018;6(9):e1019–e1027. doi:10.1016/S2214-109X(18)30329-2
18. Association WM. Wma declaration Of Helsinki – ethical principles for medical research involving human subjects. Avaialable from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
19. Katibeh M, Ziaei H, Panah E, et al. Knowledge and awareness of age related eye diseases: a population-based survey. J Ophthalmic Vis Res. 2014;9(2):223–231.
20. TheJordanTimes. Raising retirement age. Available from: https://www.jordantimes.com/opinion/fahed-fanek/raising-retirement-age.
21. Ardelia V, Jaroah S. Exploring social media use integration based on educational level among emerging adults. Int J Curr Educ Res. 2023;2(2):106–114. doi:10.53621/ijocer.v2i2.249
22. Baker P, Banks I. Men and primary care: improving access and outcomes. Eurohealth Int. 2014;20(1):22–24.
23. Sullivan DA, Rocha EM, Aragona P, et al. TFOS DEWS II Sex, Gender, and Hormones Report. Ocul Surf. 2017;15(3):284–333. doi:10.1016/j.jtos.2017.04.001
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
