Back to Journals » Clinical Ophthalmology » Volume 18
The Impact of Vergence Dysfunction on Myopia Control in Children Wearing Defocus Spectacle Lenses
Authors Ma J, Yang X, Liu Z, Fu H, Fan S, Wang K, Li Y, Huang L, Zhao M
Received 7 December 2023
Accepted for publication 28 February 2024
Published 12 March 2024 Volume 2024:18 Pages 799—807
DOI https://doi.org/10.2147/OPTH.S453731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jiahui Ma,1– 4,* Xue Yang,5,* Zhiming Liu,1– 4 Hao Fu,1– 4 Sizhou Fan,1– 4 Kai Wang,1– 4 Yan Li,1– 4 Lvzhen Huang,1– 4 Mingwei Zhao1– 4
1Department of Ophthalmology, Peking University People’s Hospital, Beijing, People’s Republic of China; 2Eye Diseases and Optometry Institute, Peking University People’s Hospital, Beijing, People’s Republic of China; 3Beijing Key Laboratory of Diagnosis and Therapy of Retinal and Choroid Diseases, Beijing, People’s Republic of China; 4College of Optometry, Peking University Health Science Center, Beijing, People’s Republic of China; 5Department of Ophthalmology, Peking University International Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kai Wang; Yan Li, Email [email protected]; [email protected]
Purpose: To investigate the impact of vergence dysfunction on myopia progression in children with Defocus incorporated multiple segments (DIMS) spectacle lenses.
Patients and Methods: We retrospectively enrolled children prescribed DIMS spectacle lenses to slow myopic progression. Baseline vergence dysfunction was determined according to phoria at distance and near. Axial length (AL) measurement and cycloplegic subjective refraction were performed before fitting the lenses and at six-month and one-year follow-ups. The six-month and one-year AL and spherical equivalent (SE) change from baseline were calculated and compared in subgroups stratified with the type of vergence dysfunction.
Results: Two hundred and ninety-two myopic children were included. Significant AL elongation and SE progression were observed at six months and one year (P < 0.05 for all comparisons). Multiple regression demonstrated that AL elongation at six months (P < 0.001) and one year (P < 0.001) was negatively correlated with age, and SE progression at six months was associated with age (P = 0.002). The AL elongation at six months in children with convergence excess was significantly greater than in normal myopic subjects (P = 0.011) and subjects with convergence insufficiency (P = 0.008), divergence excess (P = 0.007), divergence insufficiency (P = 0.024) and basic esophoria (P = 0.048) at six months.
Conclusion: The present research demonstrated that vergence dysfunction influences myopia progression for myopic children with DIMS, and the children with convergence excess suffer from the greatest myopia progression among different types of vergence dysfunction.
Keywords: myopia, vergence dysfunction, defocus spectacles, axial length
Introduction
Myopia is a prevalent ocular problem globally.1 In recent years, up to 70% of teenagers are myopic in East and Southeast Asia, and an increasing number of children have high myopia.1,2 High myopic children have higher risks of suffering from irreversible blindness-causing complications, including retinal detachment and macular diseases.3,4 Several validated interventions are applied clinically to slow myopia progression, including spectacles, contact lenses, and pharmacological treatment.5–7 Reliable evidence from animal studies has manifested that hyperopic defocus promotes axial length elongation, and myopic defocus inhibits ocular growth.8–10 Defocus incorporated multiple segments (DIMS) spectacle lenses are designed with a concentric small circular segment with relative positive power to impose myopic defocus in the mid-peripheral retina. On DIMS spectacle lenses, the defocus zone has a relatively positive power of +3.50 D. A Randomized control trial demonstrated that DIMS application slowed more than 60% axial elongation in myopic children compared with single vision spectacles wearers.11
Non-strabismic vergence dysfunction (abbreviated as vergence dysfunction) is a common optometric problem in children, which might induce visual fatigue and poor concentration.12 Among the different types of vergence dysfunction, the population-based study demonstrated that convergence insufficiency is more commonly observed than others, including convergence excess and basic exophoria.13 Previous research shows that types of refractive error were significantly associated with vergence dysfunction, including convergence and divergence insufficiency.14,15 Near positive fusional vergence is reported to be higher in myopic than emmetropia children,16 and myopes are more likely to have a higher accommodative convergence/accommodation ratio that leads toward esophoria during the near task.17 Thus, vergence dysfunction might affect the myopia progression in myopic DIMS spectacles wearer, which remains to be explored.
The present research retrospectively reviewed myopic children fitting DIMS spectacle lenses and aimed to investigate the influence of different types of vergence dysfunction on myopia progression. The study provides the basis for understanding the relationship between non-strabismic vergence dysfunction and myopia progression and might guide the myopia intervention considering the vergence dysfunction.
Materials and Methods
Study Design and Participant
The retrospective cohort study enrolled consecutive patients prescribed DIMS spectacles to slow myopia between September 2019 and 2021 at the Optometry Center of Peking University People’s Hospital. The research was conducted and adhered to the Declaration of Helsinki, and the research protocol was approved by the Peking University People’s Hospital review board. The review board exempted the informed consent due to the retrospective data collection. The patients were represented with serial numbers, and their data were confidential and preserved properly in the local database.
The inclusion criteria were as follows: (1) age between 6 and 17 years old; (2) myopia with the spherical equivalent of −1.00 to −5.00 diopters (D); (3) astigmatism and anisometropia of 2.00 D or less; (4) monocular corrected distance visual acuity (CDVA) of 20/20 Snellen chart or better; (5) first fitting DIMS spectacle lenses binocularly. The myopic children with strabismus and other ocular and systemic abnormalities were excluded. We also excluded children who applied other clinical myopia control methods simultaneously.
Intervention and Control
The myopic children in the present research wore DIMS spectacle lenses based on cycloplegic and noncycloplegic subjective refraction. The DIMS spectacle lenses consist of a 9 mm central optical zone for refractive error correction and a circular defocus zone with multiple segments. The defocus zone has a relatively positive power of +3.50 D. Each segment in the defocus zone is 1.03 mm in diameter. The DIMS spectacle lenses could provide clear distance vision and myopic defocus in the mid-peripheral retina. The children were instructed to wear the DIMS spectacle lenses full-time, except during sleep.
Ocular Examinations
Baseline ocular examinations were performed in the following order on the first day, visual acuity (standard LogMAR visual chart), slit-lamp biomicroscope, biometry (IOL master 700, Carl Zeiss Meditec AG, Jena, German) and cycloplegic automatic (Topcon KR-8100 or KR-8800, Topcon Medical System, Japan) and subjective refraction. Noncycloplegic automatic and subjective refraction and horizontal phoria at near and distance with Von Graefe method were performed on the other day. Children were followed for one month, six months and one year wearing the DIMS spectacle lenses. Visual acuity and slit-lamp biomicroscope were evaluated at each follow-up time point. Cycloplegic and noncycloplegic subjective refraction and axial length (AL) were measured at six-month and one-year follow-ups.
One drop of compound Tropicamide eye drops (Tropicamide 0.5%, phenylephrine HCL 0.5%; Sinqi Pharmaceutical, China) was instilled for cycloplegia three to four times 10 minutes apart between drops. Automatic refraction was measured as a reference for subjective refraction. For subjective refraction, fogging with a + 0.75 to + 1.50 D lens was used for accommodation relaxation. The first maximum plus to maximum VA (visual acuity) was achieved with a red-green test. We refined the cylinder axis and power with the Jackson-cross cylinder. Then, the second MPMVA was obtained to tune the spherical diopter.
Horizontal phoria at 40 cm (near) and 5 m (distance) was measured with the Von Graefe method. The optotype one size bigger than the best corrected visual acuity was chosen as the examination optotype. We used 6Δ base-up prisms to separate binocular vision and applied 12Δ base-in prisms as the measurement prism. Adjust the prism degree at the right eye until the children reported that two optotypes aligned in a single line. Then, we covered and uncovered one eye to break the fusion repeatedly and adjusted the prism degree until the children reported alignment after uncovering. The types of vergence dysfunction were defined based on the distance and near phoria measurements, and the type and diagnostic criteria are demonstrated in Table 1.14 The analyzed vergence dysfunction included convergence excess, convergence insufficiency, divergence excess, divergence insufficiency, basic esophoria and basic exophoria.
 |
Table 1 Diagnostic Criteria for Binocular Vision Dysfunction |
Statistical Analysis
SPSS software version 25.0 (IBM, Inc.) was applied for the statistical analysis. The data normality was tested with the Kolmogorov–Smirnov test. The continuous variables were described with mean and standard deviation, and categorical variables were presented as the number and percentage. Based on cycloplegic subjective refraction, the spherical equivalent (SE) was calculated as the sphere plus half of the cylinder. The SE and AL changes were calculated as the measurement at six months and one year minus the baseline.
Considering the correlation between the right and left eye, we applied the right eye data to analyze the changes of SE and AL and its influential factors. The changes of SE and AL were analyzed with a linear mixed model considering the relevance among measurements. The time point was set as the repeated factor, and the eye was set as the subject. The influential factor for SE and AL changes was analyzed with multiple linear regression.
The subgroup analysis was performed according to the types of vergence dysfunction, including normal, convergence excess, convergence insufficiency, divergence excess, divergence insufficiency, basic esophoria and basic exophoria. To investigate the impact of vergence dysfunction on myopia progression, we calculated binocular average SE and AL changes and compared them among different vergence dysfunction subgroups with the univariate linear model. Age and baseline AL and SE were adjusted as co-variate. Bonferroni correction was applied for multiple comparisons. A P value of less than 0.05 was denoted statistical significance.
Results
In total, 292 myopic children were enrolled for the analysis and the baseline demographic parameters are shown in Table 2. The mean age was 9.0 ± 2.0 years, and males accounted for 52.7% of the enrolled children. One hundred and twenty-one patients completed the one-year follow-up. At each follow-up point, all subjects showed good compliance in wearing DIMS spectacle lenses full-time and no adverse effect was observed.
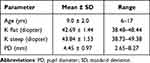 |
Table 2 Baseline Demographic Parameters |
The AL and SE at baseline, six months and one year following wearing DIMS spectacle lenses are demonstrated in Table 3. The baseline AL was 24.59 ± 0.85 mm and significantly increased to 24.71 ± 0.86 mm and 24.84 ± 0.91 mm at six months and one year, respectively. The total increase in AL over six months and one year was 0.12 ± 0.15 mm and 0.21 ± 0.21 mm, respectively. For SE, the baseline was −2.38 ± 1.42 D, and the SE decreased to −2.70 ± 1.54 D at six months and −3.03 ± 1.66 at one year. The mean myopia progression was −0.29 ± 0.46 D and −0.48 ±0.53 D over six months and one year, respectively.
 |
Table 3 Axial Length and Spherical Equivalent of the Right Eye at Baseline, Six Months and One Year Following DMIS Spectacles Wearing |
The results of influential factors analysis with the multivariate linear model are demonstrated in Table 4. The linear model demonstrates that the six-month and one-year AL elongation was significantly associated with age (P < 0.001, six months; P < 0.001, one year) and baseline SE (P < 0.001, six months; P = 0.014 one year). Six-month SE progression was significantly correlated with age (P = 0.002). Myopia progression was not found to be significantly associated with baseline AL (P > 0.05) or the magnitude of phoria (P > 0.05).
 |
Table 4 The Influential Factor Analysis for Axial Length and Spherical Equivalent Changes of the Right Eye at Six Months and One Year with the Multiple Linear Model |
The enrolled subjects were further divided into subgroups with different types of vergence dysfunction according to distance and near phoria. The demographic parameters and baseline AL and SE for subjective in different subgroups are demonstrated in Table 5. No significant difference was observed among subgroups for gender (P = 0.418), age (P = 0.337), baseline AL (P = 0.188) or baseline SE (P = 0.231).
 |
Table 5 Demographic Parameters Subgroup by the Vergence Dysfunction Type |
The AL elongation and SE progression at six months and one year for normal subjects and patients with different types of vergence dysfunction are demonstrated in Figure 1, and the data are summarized in Table 6. Adjusting for age, baseline AL and SE, the linear model demonstrated that the vergence dysfunction type was not significantly associated with AL or SE changes at six months or one year (P > 0.05 all for the analyses). Post hoc analysis showed that patients with convergence excess (0.20 ± 0.13 mm) had significantly greater AL elongation compared with normal subjects (0.13 ± 0.14 mm, P = 0.011), subjects with convergence insufficiency (0.12 ± 0.13 mm, P = 0.008), divergence excess (0.06 ± 0.12 mm, P = 0.007), divergence insufficiency (0.11 ± 0.12 mm, P = 0.024) and basic esophoria (0.13 ± 0.14 mm, P = 0.048) at six months. The subjects with divergence excess (0.25 ± 0.10 D) had significantly less SE progression compared with patients with convergence excess (−0.60 ± 0.37 D, P = 0.045), convergence insufficiency (−0.63 ± 0.66 D, P = 0.022), divergence insufficiency (−0.66 ± 0.36 D, P = 0.023) and basic esophoria (−0.54 ± 0.60 D, P = 0.033) at one year.
 |
Table 6 Axial Length and Spherical Equivalent Changes at Six Months and One Year Subgroup by the Vergence Dysfunction Type |
Discussion
DIMS could significantly slow myopia progression compared with single-vision spectacles by imposing myopic defocus in the mid-peripheral retina.11 Previous research shows that types of vergence dysfunction were correlated with refractive error. The impact of vergence dysfunction on myopia progression wearing DIMS spectacle lenses is unknown. The present research demonstrated that DIMS spectacle lenses wearers with convergence excess had faster AL elongation than normal patients and patients with other types of vergence dysfunction. The patients with divergence excess had slowed SE progression compared with subjects with other types of vergence dysfunction.
In the present research, children wearing the DIMS spectacle lenses had a mean AL elongation of 0.21 mm and SE progression of 0.48 D at one year. The result is largely consistent with several previous research.18–20Lam et al demonstrated an average AL change of 0.11 and SE change of 0.17 D at one year in a randomized clinical trial.11 The slower myopia progression in Lam et al’s study wearing DIMS spectacle lenses might be due to the difference in the age of enrolled children, which is older. Additionally, the home-based education during the COVID-19 pandemic for the children enrolled in the present study might promote myopia progression.21 The AL elongation and SE progression in the present research were smaller than the result from the study by Huang et al22 and Guo et al23 observed at one year. The children in the Huang et al study had faster myopia progression in both the DIMS and single vision spectacles group compared with the Lam et al study,11 and the author speculated that the regional disparity might be attributed to the difference.
In the present research, the influential factor analysis demonstrated that AL and SE change is significantly associated with age. The younger the children, the faster the myopia progression. The result is consistent with previous research.19,22 For younger children, the physiologic AL elongation and myopia progression are faster, which might explain the lower effect of DIMS spectacle lenses in the population. Previous research shows that DIMS spectacle lenses might retard myopia progression by altering relative peripheral refraction with the mid-periphery retinal myopic defocus.24 The relative peripheral refraction is associated with myopia onset and progression.25,26 Thus, for younger children, an increasing amount of myopic defocus might be necessary for myopia control.
Vergence dysfunction is common in children, causing blurred vision and visual fatigue.12 Types of refractive error were associated with vergence dysfunction, including convergence and divergence insufficiency.14 Thus, the type of vergence dysfunction might affect the efficiency of DIMS spectacle lenses in myopia control. The present research demonstrated that DIMS spectacle lenses wearing myopic children with convergence excess had faster AL elongation than normal myopic children and subjective with other types of vergence dysfunction. Previous studies demonstrated that accommodative convergence was greater at the onset of myopia27,28 and the near positive fusional vergence is higher in myopic than emmetropia children.16 An increasing accommodative convergence and accommodation ratio is associated with greater accommodative lag.29 Theoretically, accommodative lag might cause hyperopic defocus that weakens the effect of DIMS lenses, which induces myopia defocus in mid-peripheral retina.30 It might explain the reason for greater AL changes in DIMS spectacle lenses wearer with convergence excess. Given the result of present research, vergence dysfunction should be evaluated prior to adopting myopia control strategy.
There are certain limitations in this study. First, this is retrospective research with a high withdrawal rate, and certain confounders might influence the effect of DIMS spectacle lenses, including living habits and myopia in parents. Second, there is no control group for comparing the impact of vergence dysfunction on myopia control. A prospective controlled study is required to demonstrate the effect of vergence dysfunction on myopia progression in the future. Third, vergence dysfunction is diagnosed based on near and distance phoria. Positive and negative fusional vergence at distance and near was not assessed.
Conclusion
In conclusion, myopic subjects with convergence excess had faster AL elongation than normal myopic children and patients with other types of vergence dysfunction in DIMS wearers. Binocular vision function examination may provide crucial information in myopia control for DIMS wearers. More research is required to determine the proper use of myopia control strategy in children with different types of vergence dysfunction.
Funding
This work was funded by Chinese industry-university-research innovation foundation, new generation information technology innovation projects (2021ITA05030) and R&D foundation from Peking University People’s Hospital (RDL2022-26).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi:10.1016/j.ophtha.2016.01.006
2. Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi:10.1016/s0140-6736(12)60272-4
3. Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109(4):704–711. doi:10.1016/s0161-6420(01)01024-7
4. Cheng SC, Lam CS, Yap MK. Prevalence of myopia-related retinal changes among 12–18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt. 2013;33(6):652–660. doi:10.1111/opo.12082
5. Ha A, Kim SJ, Shim SR, Kim YK, Jung JH. Efficacy and safety of 8 atropine concentrations for myopia control in children: a network meta-analysis. Ophthalmology. 2022;129(3):322–333. doi:10.1016/j.ophtha.2021.10.016
6. Hiraoka T. Myopia control with orthokeratology: a review. Eye Contact Lens. 2022;48(3):100–104. doi:10.1097/icl.0000000000000867
7. Baird PN, Saw SM, Lanca C, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99. doi:10.1038/s41572-020-00231-4
8. Tse DY, Lam CS, Guggenheim JA, et al. Simultaneous defocus integration during refractive development. Invest Ophthalmol Visual Sci. 2007;48(12):5352–5359. doi:10.1167/iovs.07-0383
9. McFadden SA, Tse DY, Bowrey HE, et al. Integration of defocus by dual power Fresnel lenses inhibits myopia in the mammalian eye. Invest Ophthalmol Visual Sci. 2014;55(2):908–917. doi:10.1167/iovs.13-11724
10. Arumugam B, Hung LF, To CH, Holden B, Smith EL. The effects of simultaneous dual focus lenses on refractive development in infant monkeys. Invest Ophthalmol Visual Sci. 2014;55(11):7423–7432. doi:10.1167/iovs.14-14250
11. Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363–368. doi:10.1136/bjophthalmol-2018-313739
12. Scheiman M, Gallaway M, Coulter R, et al. Prevalence of vision and ocular disease conditions in a clinical pediatric population. J Am Optom Assoc. 1996;67(4):193–202.
13. Jang JU, Park IJ. Prevalence of general binocular dysfunctions among rural schoolchildren in South Korea. Taiwan J Ophthalmol. 2015;5(4):177–181. doi:10.1016/j.tjo.2015.07.005
14. Ma MM, Yeo ACH, Scheiman M, Chen X. Vergence and accommodative dysfunctions in emmetropic and myopic Chinese young adults. J Ophthalmol. 2019;2019:5904903. doi:10.1155/2019/5904903
15. Ma MM, Long W, She Z, et al. Convergence insufficiency in Chinese high school students. Clin Exp Optometry. 2019;102(2):166–171. doi:10.1111/cxo.12838
16. Jorge J, de Almeida JB, Parafita MA. Binocular vision changes in university students: a 3-year longitudinal study. Optometry Vision Sci. 2008;85(10):E999–E1006. doi:10.1097/OPX.0b013e3181890d35
17. Mutti DO, Jones LA, Moeschberger ML, Zadnik K. AC/A ratio, age, and refractive error in children. Invest Ophthalmol Visual Sci. 2000;41(9):2469–2478.
18. Nucci P, Lembo A, Schiavetti I, Shah R, Edgar DF, Evans BJW. A comparison of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) spectacles, atropine, and combined DIMS/atropine. PLoS One. 2023;18(2):e0281816. doi:10.1371/journal.pone.0281816
19. Long W, Chen K, Yu S, et al. One-year efficacy of the defocus incorporated multiple segment lens in Chinese myopic children. Optometry Vision Sci. 2023;100(1):111–116. doi:10.1097/opx.0000000000001976
20. Liu J, Lu Y, Huang D, et al. The efficacy of defocus incorporated multiple segments lenses in slowing myopia progression: results from diverse clinical circumstances. Ophthalmology. 2023;130(5):542–550. doi:10.1016/j.ophtha.2023.01.007
21. Limwattanayingyong J, Amornpetchsathaporn A, Chainakul M, Grzybowski A, Ruamviboonsuk P. The association between environmental and social factors and myopia: a review of evidence from COVID-19 pandemic. Front Public Health. 2022;10:918182. doi:10.3389/fpubh.2022.918182
22. Huang Z, Chen XF, He T, Tang Y, Du CX. Synergistic effects of defocus-incorporated multiple segments and atropine in slowing the progression of myopia. Sci Rep. 2022;12(1):22311. doi:10.1038/s41598-022-25599-z
23. Guo H, Li X, Zhang X, Wang H, Li J. Comparing the effects of highly aspherical lenslets versus defocus incorporated multiple segment spectacle lenses on myopia control. Sci Rep. 2023;13(1):3048. doi:10.1038/s41598-023-30157-2
24. Zhang HY, Lam CSY, Tang WC, Lee PH, Tse DY, To CH. Changes in relative peripheral refraction in children who switched from single-vision lenses to Defocus Incorporated Multiple Segments lenses. Ophthalmic Physiol Opt. 2022. doi:10.1111/opo.13086
25. Mutti DO, Sinnott LT, Mitchell GL, et al. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest Ophthalmol Visual Sci. 2011;52(1):199–205. doi:10.1167/iovs.09-4826
26. Choi KY, Mok AY, Do CW, Lee PH, Chan HH. The diversified defocus profile of the near-work environment and myopia development. Ophthalmic Physiol Opt. 2020;40(4):463–471. doi:10.1111/opo.12698
27. Gwiazda J, Thorn F, Held R. Accommodation, accommodative convergence, and response AC/A ratios before and at the onset of myopia in children. Optometry Vision Sci. 2005;82(4):273–278. doi:10.1097/01.opx.0000159363.07082.7d
28. Goss DA, Jackson TW. Clinical findings before the onset of myopia in youth: 3. Heterophoria. Optometry Vision Sci. 1996;73(4):269–278. doi:10.1097/00006324-199604000-00009
29. Mutti DO, Mitchell GL, Jones-Jordan LA, et al. The response AC/A ratio before and after the onset of myopia. Invest Ophthalmol Visual Sci. 2017;58(3):1594–1602. doi:10.1167/iovs.16-19093
30. Zhang HY, Lam CSY, Tang WC, Leung M, To CH. Defocus incorporated multiple segments spectacle lenses changed the relative peripheral refraction: a 2-year randomized clinical trial. Invest Ophthalmol Visual Sci. 2020;61(5):53. doi:10.1167/iovs.61.5.53
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Visual Acuity Prior to Cataract Surgery and Risk of Retinal Detachment – A Population-Based Study
Thylefors J, Jakobsson G, Zetterberg M, Sheikh R
Clinical Ophthalmology 2023, 17:1975-1980
Published Date: 12 July 2023

