Back to Journals » Drug Design, Development and Therapy » Volume 18
The Role of Plasma Trough Concentration of Voriconazole and Voriconazole N-Oxide in Its Hepatotoxicity in Adult Patients
Authors Cheng L , You X, Wang X, Yu M, Jia C
Received 26 April 2024
Accepted for publication 9 August 2024
Published 13 August 2024 Volume 2024:18 Pages 3617—3628
DOI https://doi.org/10.2147/DDDT.S475706
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Anastasios Lymperopoulos
Lin Cheng, Xi You, Xiaowen Wang, Mingjie Yu, Changsheng Jia
Department of Pharmacy, the First Affiliated Hospital of Army Medical University, Chongqing, People’s Republic of China
Correspondence: Lin Cheng; Mingjie Yu, Email [email protected]; [email protected]
Objective: Hepatotoxicity is an important cause of early withdrawal of voriconazole (VCZ). The role of the plasma trough concentration of VCZ (C0) in hepatotoxicity is confusion. VCZ N-oxide is the primary metabolite of VCZ in plasma. We investigated the role of VCZ C0 and plasma trough concentration of VCZ N-oxide (CN) in hepatotoxicity in adult patients.
Materials and Methods: This was a prospective study. VCZ C0 and CN were measured using liquid chromatography-tandem mass spectrometry.
Results: In total, 601 VCZ C0 and CN from 376 adult patients were included. The percentage of grade 1 or higher adverse events for ALP, ALT, AST, γ-GT, and TBIL were 35.4%, 21.0%, 30.1%, 56.2%, and 22.2%, respectively. Compared with younger adult patients, elderly patients (≥ 65 years) had a higher rate of grade 1 or higher adverse events of ALP. In the multivariate analysis, VCZ C0 was a risk factor for grade 1 or higher adverse events of AST in elderly patients and TBIL in younger adult patients, and VCZ CN was a risk factor for grade 1 or higher adverse events of ALT, AST, and TBIL. Results of the receiver operating characteristic curve analysis indicated that when the VCZ C0 was higher than 4.0 μg/mL, or the VCZ CN was lower than 1.7 μg/mL, the incidence of grade 1 or higher adverse events of AST and TBIL increased.
Conclusion: VCZ C0 and CN were associated with liver function-related adverse events. Measurement of VCZ CN should be considered for VCZ therapeutic drug monitoring.
Keywords: voriconazole, voriconazole N-oxide, hepatotoxicity, therapeutic drug monitoring
Introduction
Voriconazole (VCZ), a broad-spectrum triazole antifungal drug, is widely used to prevent and treat invasive fungal infections (IFIs) caused by Aspergillus and Candida.1 Compared with other triazole antifungal drugs such as isavuconazole and posaconazole for the treatment of IFIs, VCZ has similar therapeutic and preventive effects; however, the incidence of adverse events caused by VCZ is higher than that of isavuconazole and posaconazole.2–4 According to the FDA Adverse Reaction Reporting System data from the first quarter of 2004 to the third quarter of 2021, the incidence of drug-induced liver injury (DILI) caused by antifungal drugs was 32.45% for VCZ.5 Studies have also shown that the overall incidence of adverse events associated with VCZ in the treatment of IFIs is 40%, and common adverse events include elevated glutamic-pyruvic transaminase (ALT), glutamic-oxaloacetic transaminase (AST), alkaline phosphatase (ALP), and γ-glutamyl transferase (γ-GT), as well as an increase in hallucinations, nausea, and blurred vision.4 In allogeneic hematopoietic stem cell transplantation recipients, adverse events accounted for 68.7% of the early discontinuation of VCZ,6 and liver toxicity was an important reason for the early withdrawal of VCZ, accounting for 22.8%.4 Our previous study also showed that the incidence of abnormal liver function indicators among the adverse events caused by VCZ was 49.3% in elderly patients and 37.6% in younger adult patients.7 Therefore, it is important to investigate factors associated with VCZ-induced hepatotoxicity for rational use.
Previous studies have suggested a correlation between the plasma trough concentration of VCZ (C0) and adverse events, and monitoring of VCZ C0 has long been suggested to optimize its effectiveness and minimize toxicity.8,9 However, these results remain confusion. The therapeutic window of VCZ recommended for most European patients is a trough level of 1–5.5 μg/mL,1 which for Chinese patients is in the range of 0.5–5 μg/mL.10 In a systematic review and meta-analysis, the incidence of hepatotoxicity was significantly increased with VCZ C0>3.0, >4.0, >5.5 and >6.0 μg/mL.8 In another systematic review and meta-analysis, the highest odds ratios for a significantly higher risk of hepatotoxicity were recorded at 4.0 μg/mL.11 Steady-state VCZ C0>3.61 μg/mL has also been reported to be associated with an increased incidence of hepatotoxicity in patients with pulmonary fungal diseases.12 Furthermore, a lack of correlation between the serum VCZ level and the occurrence of hepatotoxicity has been observed in many patients.13,14
VCZ is mainly metabolized in the liver by isoenzymes cytochrome P450 2C19 (CYP2C19), CYP3A4, and CYP2C9. VCZ N-oxide is the primary metabolite of VCZ in the plasma.15 Thus, the plasma concentration of VCZ N-oxide (CN) and the ratio of VCZ CN/C0 may reflect the patient’s metabolic capacity and liver function at a given time and have the potential to predict VCZ-induced hepatotoxicity. In the current study, we investigated the role of VCZ C0, CN, and CN/C0 in adverse events of liver function in adult patients. The basic characteristics of patients, fungal test results, administration route and dose of VCZ, duration of VCZ administration, VCZ C0, CN, and CN/C0, combined use of drugs, and laboratory test results, such as inflammatory indicators, renal function indicators, blood routine indicators, and electrolyte indicators, were included as influencing factors of adverse events of liver function. Considering the impaired liver function in the elderly16 and limited data on VCZ-induced hepatotoxicity in the elderly, we also investigated factors associated with VCZ-induced hepatotoxicity in elderly patients (≥65 years).
Materials and Methods
Patients and Study Design
This single-center prospective study included adult patients receiving VCZ therapeutic drug monitoring in the Southwest Hospital of Chongqing from January 2021 to December 2023. Both patients with prophylactic and therapeutic uses of VCZ were included. The inclusion criteria for the patients were as follows: (a) receiving VCZ either intravenously or orally; (b) the measured VCZ C0was under the steady state. In the case of the loading dose (6 mg/kg intravenously or 400 mg orally), the stable VCZ C0 was achieved at the end of the second day of administration and before the fifth administration (day 3). In the absence of loading doses, VCZ C0 was measure on day 5 or later;10 (c) available liver function results in the early stage of administration, and the results measured on the same day of VCZ C0 determination; (d) agreed to the use of their blood samples for VCZ CN determination; and (e) signed informed consent forms. The exclusion criteria were (a) abnormal liver function before VCZ administration and (b) current pregnancy.
Data Collection
The following data were collected for each patient: (a) demographic characteristics, including age, sex, weight, underlying diseases, and fungal test results; (b)medication information, including VCZ dose and administration route, duration of VCZ administration, and combined use of antibiotics, corticosteroids, and proton-pump inhibitors (PPIs); (c) liver function indicators, including ALP, ALT, AST, γ-GT, and total bilirubin (TBIL); (d) inflammatory indicators, including procalcitonin (PCT) and interleukin 6 (IL-6); (e) kidney function, including serum creatinine, blood urea nitrogen (BUN), and estimated glomerular filtration rate (eGFR); (f) blood count, including white blood cells (WBC), red blood cells (RBC), hemoglobin (Hb), platelet count (PLT), mean platelet volume (MPV), platelet distribution width (PDW), hematocrit (HCT) and platelet hematocrit; (g) and serum potassium, sodium and chloride levels.
VCZ C0 and CN Determination
VCZ CN was measured together with VCZ C0 using liquid chromatography-tandem mass spectrometry as previously described.17 The limits of detection of VCZ C0 and CN were 8 and 10ng/mL, respectively. The lower limits of quantification for VCZ C0 and CN were 400 ng/mL.
Statistical Analysis
Statistical analysis was performed using IBM SPSS (version 26.0; IBM Corp., Armonk, NY, USA). Categorical data were compared using the chi-square test. Data conforming to a normal distribution from the two cohorts were compared using independent-sample t-tests. Data that did not conform to a normal distribution from the two cohorts were represented by the median and interquartile range (IQR) and compared using the Mann–Whitney U-test. The Common Terminology Criteria for Adverse Events (CTCAE) 5.0 was used to grade hepatotoxicity. The criteria for grade 1, 2, 3, and 4 adverse effects of ALT and AST were respectively >1.0–3.0×upper limit of normal (ULN), >3.0–5.0×ULN, >5.0–20.0×ULN, and >20.0×ULN. The criteria for grade 1, 2, 3, and 4 adverse effects of ALP and γ-GT were respectively >1.0–2.5×ULN, >2.5–5.0×ULN, >5.0–20.0×ULN, and >20.0×ULN. The criteria for grade 1, 2, 3, and 4 adverse effects of TBIL were respectively >1.0–1.5×ULN, >1.5–3.0×ULN, >3.0–10.0×ULN, and >10.0×ULN. Binary logistic regression was used to evaluate the risk factors for grade 1 or higher adverse events of ALP, ALT, AST, γ-GT, and TBIL levels. Covariates with a p value of <0.1 in the univariate analysis, were entered into the multivariate analysis. Receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive effect of VCZ C0 and CN on adverse events of liver function. Statistical significance was set at p<0.05.
Results
Patient Characteristics
A total of 601 VCZ C0 and CN from 376 adult patients were included, including 383 VCZ C0 and CN from 248 younger adult patients, and 218 VCZ C0 and CN from 128 elderly patients (Table 1). Male patients accounted for 62.0% of the patients. Pneumonia and hematological malignancies were the primary baseline diseases. Approximately one-third of the patients had negative fungal detection results. Most patients had combined use of antibiotics, and one-third of the patients received corticosteroids and PPIs. The major route of administration of VCZ is via intravenous administration. The median time for VCZ C0 and CN measurements was 8 days after VCZ administration. The median values of VCZ C0, CN and CN/ C0 were 3.41 μg/mL, 2.10 μg/mL and 0.74, respectively.
 |
Table 1 Demographic and Clinical Characteristics of Patients |
The proportion of men in the elderly patients was significantly higher than that in the younger adult patients (p<0.05). The VCZ dose in the elderly patients was significantly lower than that in the younger adult patients (p<0.05). The time for C0 and CN measurements after VCZ administration in the elderly patients was longer than that in the younger adult patients (p<0.05). The VCZ C0 and CN in the two cohorts were similar (p>0.05), but a lower VCZ CN/C0 was observed in the elderly patients (p<0.05).
The main antibiotics employed in combination were imipenem-cilastatin, cephalosporins, meropenem, cefoperazone, vancomycin, piperacillin, tigecycline, teicoplanin, levofloxacin, and moxifloxacin (Table 2). The proportion of the combined use of cephalosporins, cefoperazone, and levofloxacin in elderly patients was higher than that in younger adult patients, while the proportion of the combined use of imipenem-cilastatin and vancomycin in elderly patients was lower (p<0.05). The proportion of the combined use of antibiotics with potential hepatotoxicity in elderly patients, including cefoperazone, piperacillin, tigecycline, metronidazole, compound sulfamethoxazole, minocycline, and roxithromycin, was higher than that in younger adult patients (44.0% vs 35.2%, p=0.033).
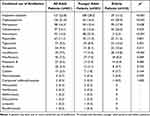 |
Table 2 The Combined Use of Antibiotics in Patients |
The percentage of grade 1 or higher adverse events for ALP, ALT, AST, γ-GT, and TBIL were 35.4%, 21.0%, 30.1%, 56.2%, and 22.2%, respectively. Compared with younger adult patients, elderly patients had a higher rate of grade 1 or higher adverse events of ALP (Table 3).
 |
Table 3 Distribution of Adverse Events of Liver Function in Patients |
Risk Factors of Grade 1 or Higher Adverse Events of Liver Function
A total of 27 factors were incorporated in the univariate analysis, encompassing sex, age, fungal test results, VCZ dose, route of VCZ administration, VCZ C0, CN, and CN/C0, duration of VCZ treatment, combined use of antibiotics with potential hepatotoxicity and PPIs, levels of IL-6 and PCT, serum creatinine, BUN, eGFR, WBC, RBC, Hb, PLT, MPV, PDW, HCT, platelet hematocrit, serum potassium, sodium and chloride levels. Risk factors for grade 1 or higher adverse events of liver function (p<0.1) in the univariate analysis were shown in Figures 1–3. In the multivariate analysis, VCZ dose was a risk factor for grade 1 or higher adverse events of ALP and TBIL; duration of VCZ treatment was a risk factor for grade 1 or higher adverse events of ALP, ALT, and γ-GT; VCZ C0 was a risk factor for grade 1 or higher adverse events of AST in elderly patients and TBIL in younger adult patients; and VCZ CN was a risk factor for grade 1 or higher adverse events of ALT, AST, and TBIL. In addition, sex, combined use of PPIs and antibiotics with hepatotoxicity, MPV, PDW, RBC, Hb, serum sodium and chloride, BUN, and IL-6 were also identified as risk factors for grade 1 or higher adverse events of liver function (Table 4).
 |
Table 4 Risk Factors for Adverse Events of Liver Function in Patients |
 |
Figure 1 Risk factors for grade 1 or higher adverse events of liver function in all adult patients (p<0.1 in univariate analysis). (A) ALP, (B) ALT, (C) AST, (D) γ-GT, and (E) TBIL. |
 |
Figure 2 Risk factors for grade 1 or higher adverse events of liver function in younger adult patients (p<0.1 in univariate analysis). (A) ALP, (B) ALT, (C) AST, (D) γ-GT, and (E) TBIL. |
 |
Figure 3 Risk factors for grade 1 or higher adverse events of liver function in elderly patients (p<0.1 in univariate analysis). (A) ALP, (B) ALT, (C) AST, (D) γ-GT, and (E) TBIL. |
Prediction Value of VCZ C0 and CN for Grade 1 or Higher Adverse Events of Liver Function
In younger adult patients, the results of the ROC curve analysis indicated that when VCZ C0 levels of ≥4.04 μg/mL and VCZ CN levels of <1.71 μg/mL, the incidence of grade 1 or higher adverse events of TBIL increased (Figure 4A and B). In elderly patients, the results of the ROC curve analysis indicated that when VCZ C0 levels of ≥4.26 μg/mL and VCZ CN levels of <1.70 μg/mL, the incidence of grade 1 or higher adverse events of AST increased (Figure 4C and D).
Discussion
VCZ is an important drug for the treatment of IFIs, especially those caused by Aspergillus. Hepatotoxicity has become an important cause of early withdrawal of VCZ, and VCZ C0 has been suggested to be associated with hepatotoxicity. VCZ CN is not routinely monitored in the clinic, and its role in hepatotoxicity remains unknown. In this study, we investigated the role of VCZ C0 and CN in its hepatotoxicity in adult patients. The median VCZ C0 and CN in our study were slightly higher than the values reported in two Japanese studies but with similar CN/C0.18,19 VCZ CN/C0 was reported to be lower in Japanese patients who receiving VCZ with intravenous, with higher levels of C-reactive protein on the same day as VCZ C0 measurement, CYP2C19 extensive metabolizer, and with old age.18 Our previous study also showed that for patients with CYP2C19 normal metabolizer, VCZ C0, C0/dose, and C0/CN were significantly higher in the elderly patients.17 The values of VCZ CN/C0 in younger adult patients and elderly patients in the current study were consistent with the results of previous studies.
To decrease VCZ-associated adverse events, C0<4.0 µg/mL is strongly recommended for Asians, whereas C0<5.5 µg/mL is generally recommended for non-Asians.20 One study reported a significant difference in hepatotoxicity between patients with VCZ C0≥ 4 µg/mL and those with VCZ C0< 4 µg/mL.21,22 In another study, liver enzyme abnormality was observed in 34.5% of patients with VCZ C0> or = 3.9 µg/mL.23 Similar results were also observed in our study. The cut off value of VCZ C0 for grade 1 or higher adverse events of TBIL was 4.04 μg/mL in younger adult patients, while the cut off value of VCZ C0 for grade 1 or higher adverse events of AST was 4.26 μg/mL in elderly patients.
In Yamada’s study, VCZ CN was correlated with a serum TBIL concentration.19 We observed that VCZ CN was a risk factor for grade 1 or higher adverse events of TBIL, ALT, and AST. Interestingly, the cutoff values of VCZ CN for grade 1 or higher adverse events of TBIL in younger adult patients and for grade 1 or higher adverse events of AST in elderly patients were both 1.7 μg/mL. In general, when VCZ C0 was higher than 4.0 μg/mL, or VCZ CN was lower than 1.7 μg/mL, the incidence of grade 1 or higher adverse events of AST and TBIL increased. To the best of our knowledge, this is the first report of VCZ CN as a risk factor for adverse events of liver function.
A previous study showed that hepatotoxicity occurred in 66.7% of patients within 7 days of the first dose of VCZ and in 94.4% within 15 days of the dose.12 In another study, hepatotoxicity occurred in 6.0% of the patients after a median of 10 days.24 Wang et al reported that the median time to hepatotoxicity was 3 days (range 1–24 days), and 83.2% of hepatotoxicity cases occurred within 7 days of VCZ initiation.25 Taghvaye-Masoumi et al reported that only VCZ C0 on day 14 is associated with hepatotoxicity.26 We also found that the duration of VCZ administration was associated with grade 1 or higher adverse events of ALP, ALT, and γ-GT.
In the current study, approximately 84% of patients received antibiotics when using VCZ, which had potential hepatotoxicity or nephrotoxicity. PPIs are metabolized by the CYP2C19, CYP3A4, and CYP2C9 enzymes in the liver. The combined use of PPIs and VCZ can affect the C0. We found that the combined use of antibiotics with hepatotoxicity and PPIs were risk factors for grade 1 or higher adverse events of ALT and γ-GT in elderly patients, which may be attributed to the higher proportion of combined use of antibiotics with hepatotoxicity, as well as the decreased CYP enzymes in these patients. To decrease the incidence of VCZ-associated adverse events of liver function in elderly patients, it is better not to combine antibiotics with potential hepatotoxicity. In addition, sex, MPV, PDW, RBC, Hb, serum sodium and chloride, BUN, and IL-6 levels were also associated with grade 1 or higher adverse events of liver function in our study, which should be considered when using VCZ.
This study has some limitations. First, it was a monocenter study, which could have led to a bias in the analysis. Second, pharmacogenetic data of patients were not included in the analysis, such as drug-metabolizing enzymes and genotype of CYP2C19. However, the effect of CYP2C19 genotypes on the incidence of adverse effects of VCZ has not been confirmed.19,27,28 Based on our results, the risk of hepatotoxicity can be predicted by determining VCZ C0 and CN. Finally, since numerous variables demonstrated an influence on grade 1 or higher adverse events of liver function, VCZ C0 and CN ought to be combined with other indicators for thorough consideration when evaluating potential hepatotoxicity.
Conclusion
In summary, we report for the first time that VCZ CN is a risk factor for its hepatotoxicity. Hepatotoxicity is more prevalent in the Asian population. The measurement of VCZ CN may provide additional useful information in the early phase of liver injury. VCZ C0 and CN should be monitored as early as the steady state concentration is achieved to avoid hepatotoxicity. It is possible to predict the onset of liver damage in advance. In practice, the VCZ CN assay is relatively easy and inexpensive. It is necessary to determine VCZ CN in VCZ therapeutic drug monitoring to limit its hepatotoxicity.
Data Sharing Statement
The original contributions presented in this study are included in the article, and further inquiries can be directed to the corresponding author.
Ethical Statement
This study was approved by the Ethics Committee of the First Affiliated Hospital of the Army Medical University (approval number: KY2023104). All organs were donated voluntarily with written informed consent, and that these were conducted in accordance with the Declaration of Istanbul.
Funding
This work was supported by the General Program of the Chongqing Natural Science Foundation (CSTB2023NSCQ-MSX0622), the Medical Research Project of Science and Health of Chongqing (2023MSXM124), and Key Specialty of Clinical Pharmacy of Chongqing, China.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Ullmann AJ, Aguado JM, Arikan-Akdagli S, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline.. Clin Microbiol Infec. 2018;24 Suppl 1(1):e1–e38. doi:10.1016/j.cmi.2018.01.002
2. Maertens JA, Rahav G, Lee DG, et al. Posaconazole versus voriconazole for primary treatment of invasive aspergillosis: a Phase 3, randomised, controlled, non-inferiority trial. Lancet. 2021;397:499–509. doi:10.1016/S0140-6736(21)00219-1
3. Samanta P, Clancy CJ, Marini RV, et al. Isavuconazole is as effective as and better tolerated than voriconazole for antifungal prophylaxis in lung transplant recipients. Clin Infect Dis. 2021;73:416–426. doi:10.1093/cid/ciaa652
4. Bogler Y, Stern A, Su Y, et al. Efficacy and safety of isavuconazole compared with voriconazole as primary antifungal prophylaxis in allogeneic hematopoietic cell transplant recipients. Med Mycol. 2021;59:970–979. doi:10.1093/mmy/myab025
5. Zhou ZX, Yin XD, Zhang Y, et al. Antifungal drugs and drug-induced liver injury: a real-world study leveraging the FDA adverse event reporting system database. Front Pharmacol. 2022;13:891336. doi:10.3389/fphar.2022.891336
6. Chan SY, Hughes RM, Woo K, Perales MA, Neofytos D, Papanicolaou G. Reasons for voriconazole prophylaxis discontinuation in allogeneic hematopoietic cell transplant recipients: a real-life paradigm. Med Mycol. 2020;58:1029–1036. doi:10.1093/mmy/myaa008
7. Cheng L, Xiang R, Liu F, et al. Therapeutic drug monitoring and safety of voriconazole in elderly patients. Int Immunopharmacol. 2020;78:106078. doi:10.1016/j.intimp.2019.106078
8. Jin H, Wang T, Falcione BA, et al. Trough concentration of voriconazole and its relationship with efficacy and safety: a systematic review and meta-analysis. J Antimicrob Chemother. 2016;71:1772–1785. doi:10.1093/jac/dkw045
9. Patterson TF, Thompson GR, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;63:e1–e60. doi:10.1093/cid/ciw326
10. Chen K, Zhang X, Ke X, Du G, Yang K, Zhai S. Individualized medication of voriconazole: a practice guideline of the division of therapeutic drug monitoring, Chinese Pharmacological Society. Therapeut Drug Monit. 2018;40:663–674. doi:10.1097/FTD.0000000000000561
11. Hanai Y, Hamada Y, Kimura T, et al. Favorable effects of voriconazole trough concentrations exceeding 1 mug/mL on treatment success and all-cause mortality: a systematic review and meta-analysis. J Fungi. 2021;7:306. doi:10.3390/jof7040306
12. Shen K, Gu Y, Wang Y, et al. Therapeutic drug monitoring and safety evaluation of voriconazole in the treatment of pulmonary fungal diseases. Therap Advan Drug Saf. 2022;13:20420986221127503. doi:10.1177/20420986221127503
13. Mihaila RG. Voriconazole and the liver. World J Hepatol. 2015;7:1828–1833. doi:10.4254/wjh.v7.i14.1828
14. Zonios D, Yamazaki H, Murayama N, et al. Voriconazole metabolism, toxicity, and the effect of cytochrome P450 2C19 genotype. J Infect Dis. 2014;209:1941–1948. doi:10.1093/infdis/jiu017
15. Geist MJ, Egerer G, Burhenne J, Riedel KD, Weiss J, Mikus G. Steady-state pharmacokinetics and metabolism of voriconazole in patients. J Antimicrob Chemother. 2013;68:2592–2599. doi:10.1093/jac/dkt229
16. K-C W, Lin C-J. The regulation of drug-metabolizing enzymes and membrane transporters by inflammation: evidences in inflammatory diseases and age-related disorders. J Food Drug Analy. 2019;27:48–59. doi:10.1016/j.jfda.2018.11.005
17. Shang S, Cheng L, Li X, et al. Effect of CYP2C19 polymorphism on the plasma voriconazole concentration and voriconazole-to-voriconazole-N-oxide concentration ratio in elderly patients. Mycoses. 2020;63:1181–1190. doi:10.1111/myc.13105
18. Niioka T, Fujishima N, Abumiya M, et al. Relationship between the CYP2C19 phenotype using the voriconazole-to-voriconazole N-oxide plasma concentration ratio and demographic and clinical characteristics of Japanese patients with different CYP2C19 genotypes. Therapeut Drug Monit. 2017;39:514–521. doi:10.1097/FTD.0000000000000441
19. Yamada T, Mino Y, Naito T, Kawakami J. Impact of flavin-containing monooxygenase 3 and CYP2C19 genotypes on plasma disposition and adverse effects of voriconazole administered orally in immunocompromised patients. J Infect Chemoth. 2019;25:1019–1025. doi:10.1016/j.jiac.2019.05.032
20. Takesue Y, Hanai Y, Oda K, et al. Japanese antimicrobial therapeutic drug monitoring guideline C. Clinical practice guideline for the therapeutic drug monitoring of voriconazole in non-Asian and Asian adult patients: consensus review by the Japanese Society of Chemotherapy and the Japanese society of therapeutic drug monitoring. Clin Ther. 2022;44:1604–1623. doi:10.1016/j.clinthera.2022.10.005
21. Wang Y, Wang T, Xie J, et al. Risk factors for voriconazole-associated hepatotoxicity in patients in the intensive care unit. Pharmacotherapy. 2016;36:757–765. doi:10.1002/phar.1779
22. Suzuki Y, Tokimatsu I, Sato Y, et al. Association of sustained high plasma trough concentration of voriconazole with the incidence of hepatotoxicity. Int J Clin Chem. 2013;424:119–122. doi:10.1016/j.cca.2013.05.025
23. Matsumoto K, Ikawa K, Abematsu K, et al. Correlation between voriconazole trough plasma concentration and hepatotoxicity in patients with different CYP2C19 genotypes. Int J Antimicrob Agents. 2009;34:91–94. doi:10.1016/j.ijantimicag.2009.01.008
24. Hamada Y, Ueda T, Miyazaki Y, et al. Effects of antifungal stewardship using therapeutic drug monitoring in voriconazole therapy on the prevention and control of hepatotoxicity and visual symptoms: a multicentre study conducted in Japan. Mycoses. 2020;63:779–786. doi:10.1111/myc.13129
25. Wang T, Miao L, Shao H, et al. Voriconazole therapeutic drug monitoring and hepatotoxicity in critically ill patients: a nationwide multi-centre retrospective study. Int J Antimicrob Agents. 2022;60:106692. doi:10.1016/j.ijantimicag.2022.106692
26. Taghvaye-Masoumi H, Hadjibabaie M, Ghadimi M, Zarif-Yeganeh M, Vaezi M, Ghavamzadeh A. Association of voriconazole trough plasma concentration with efficacy and incidence of hepatotoxicity in Iranian patients with hematological malignancies. Iran J Pharmac Res. 2021;20:62–71. doi:10.22037/ijpr.2020.112330.13688
27. Lee J, Ng P, Hamandi B, Husain S, Lefebvre MJ, Battistella M. Effect of therapeutic drug monitoring and cytochrome P450 2C19 genotyping on clinical outcomes of voriconazole: a systematic review. Anna Pharmacoth. 2021;55:509–529. doi:10.1177/1060028020948174
28. Li X, Yu C, Wang T, Chen K, Zhai S, Tang H. Effect of cytochrome P450 2C19 polymorphisms on the clinical outcomes of voriconazole: a systematic review and meta-analysis. Eur J Clin Pharmacol. 2016;72:1185–1193. doi:10.1007/s00228-016-2089-y
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

