Back to Journals » Advances in Medical Education and Practice » Volume 15
Assessing the Proficiency in Basic and Advanced Life Support Among Physicians in Ecuador: A Cross-Sectional Study
Authors Izquierdo-Condoy JS , Naranjo-Lara P, Arias Rodríguez FD, Puglla-Mendoza AG, Jima-Sanmartín J, Andrade Casanova D, Duque-Sánchez EP, Alegría N N, Rojas Cadena MG, Ortiz-Prado E
Received 10 October 2023
Accepted for publication 14 December 2023
Published 6 January 2024 Volume 2024:15 Pages 25—35
DOI https://doi.org/10.2147/AMEP.S440437
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Juan S Izquierdo-Condoy,1 Patricio Naranjo-Lara,1 Fabián D Arias Rodríguez,2 Alexander Gilberto Puglla-Mendoza,1 Jackson Jima-Sanmartín,1 Dayana Andrade Casanova,1 Erick Patricio Duque-Sánchez,1 Nicolás Alegría N,1 Marlon Guillermo Rojas Cadena,1 Esteban Ortiz-Prado1
1One Health Research Group, Faculty of Medicine, Universidad de las Américas, Quito, Ecuador; 2Área de Gestión de Docencia e Investigación, Hospital Pediátrico Baca Ortiz, Quito, Ecuador
Correspondence: Esteban Ortiz-Prado, One Health Research Group, Universidad de las Américas, Ecuador Calle de los Colimes y Avenida De los Granados, Quito, 170137, Ecuador, Tel +593995760693, Email [email protected]
Purpose: Cardiorespiratory arrest’s unpredictability poses a global health challenge, with gaps in physicians’ life support knowledge potentially leading to poor patient outcomes, a factor yet unstudied among Ecuadorian physicians. This study aims to elucidate the state of physicians’ theoretical knowledge in Ecuador based on Basic Life Support (BLS) and Advanced Life Support (ALS) guidelines.
Patients and methods: A national cross-sectional online 35-questions survey was conducted between February and March 2023 using a self-administered, expert-validated questionnaire. Participants’ responses were obtained through official social media groups (WhatsApp and Facebook). The survey evaluated the theoretical knowledge of BLS and ALS, with scores based on the number of correct answers out of a maximum of 10.0 points. For descriptive analysis, frequencies, percentages, means, and standard deviations (SD) were used. The T-test and one-way ANOVA were utilized to analyze the associations between knowledge levels and demographic and academic training variables of Ecuadorian doctors. Values of p < 0.05 were considered statistically significant for all analyses.
Results: The survey garnered responses from 385 physicians, with a majority being female (56.6%) and possessing less than 3 years of work experience (75.1%). Of these, 71.7% and 51.9% held BLS and ALS certifications, respectively. Knowledge scores for BLS (5.8/10 ± 1.6) surpassed those for ALS (4.7/10 ± 1.8) (p < 0.001). Physicians with less than 3 years of work experience exhibited higher knowledge scores in both BLS and ALS tests (p < 0.05).
Conclusion: This study revealed a notable deficiency in the theoretical knowledge of BLS and ALS among surveyed Ecuadorian physicians. Factors such as prior certification and years of work experience appeared to influence knowledge levels. Continual training and updates in life support protocols at universities and healthcare institutions are key to enhancing physicians’ skills and patient outcomes.
Keywords: cardiopulmonary resuscitation, knowledge, education, medical, physicians
Introduction
Cardiorespiratory arrest, defined as an abrupt and unexpected cessation of heart function and spontaneous breathing, is potentially reversible, albeit catastrophic if not promptly addressed.1,2 While the heart exhibits a relatively high tolerance to anoxia, the central nervous system suffers irreparable damage after 3 to 4 minutes of oxygen deprivation. Hence, immediate and effective resuscitation, underpinned by sound theoretical and practical knowledge, is of paramount importance.3 According to the World Health Organization (WHO) (2015), cardiopulmonary arrest accounts for over 60% of ischemic heart disease fatalities.4 In contemporary medical practice, Cardiopulmonary Resuscitation (CPR) is viewed as a series of maneuvers designed to reverse cardiorespiratory arrest. The primary goal is to substitute and subsequently restore spontaneous breathing and circulation to avert death from irreversible damage to vital organs, primarily the brain.5 With the evolution of CPR, two resuscitation frameworks, Basic Life Support (BLS) and Advanced Life Support (ALS), have been established. The American Heart Association (AHA) periodically updates these BLS and ALS guidelines to optimize patient outcomes.6
BLS maneuvers, while conceptually straightforward, focus on promoting systemic blood flow via thoracic compression and maintaining blood oxygenation. The quality of these maneuvers is pivotal to successful resuscitation.2,7 Conversely, ALS encompasses more technically intricate maneuvers targeting the remaining links in the chain of survival, including rapid defibrillation and post-resuscitation care. ALS is typically conducted in hospital settings.7 Effective training in both BLS and ALS is crucial for any healthcare system aiming to mitigate the severe impacts of cardiorespiratory arrest. Studies reveal that in-hospital and out-of-hospital cardiac arrest survival rates in developed countries stand at 17.6% and a dismal 6.4%, respectively.8 The quality of resuscitation plays a crucial role in these outcomes. Lower survival rates are linked to ineffective resuscitation; however, when performed by trained professionals, BLS can improve survival rates by 7 to 24%.9–12 Recent research has highlighted a deficiency in physicians’ understanding of basic and advanced cardiopulmonary resuscitation.13,14 Despite investigations in North America, Europe, and Africa, information regarding the comprehension of life support techniques in South America is scarce.
Methods
Study Question and Objectives
This study was developed using a testing strategy based on objectively describing a measurable phenomenon. Our research question was: What is the level of theoretical knowledge about BLS and ALS among Ecuadorian physicians?
Therefore, the primary objective of this study is to explore the theoretical understanding of BLS and ALS among doctors in Ecuador. Additionally, the secondary objectives of this research are: 1) identify the state of training and preparation in BLS and ALS among Ecuadorian physicians, 2) examining differences in the level of theoretical knowledge of BLS and ALS among Ecuadorian physicians based on demographic characteristics, and 3) evaluating differences in the level of theoretical knowledge of BLS and ALS among Ecuadorian physicians according to training variables.
Study Design
We conducted a descriptive, cross-sectional, nationwide study utilizing a 35-question online survey to gather information from volunteer Ecuadorian physicians.
Setting and Participants
Between January 2023 and March 2023, an online survey was executed, targeting graduate physicians based in Ecuador. A convenience, non-probabilistic sampling method was used for participant selection.
Data Measurement and Questionnaire
Our research team crafted a comprehensive questionnaire to evaluate Ecuadorian physicians’ knowledge of BLS and ALS. We formulated questions about the theoretical underpinnings of basic and advanced life support, drawing from the questionnaire developed by Passali et al,13 the AHA guidelines for BLS and ALS in their 2020 update,6 and the demographic and work characteristics of the participants.
Prior to full-scale deployment, we conducted a pilot study with 20 Ecuadorian physicians to detect potential comprehension issues or questionnaire design errors. Based on feedback from the pilot study, we revised several questions and finalized a 35-item Spanish questionnaire. This questionnaire was subsequently validated by three emergency medicine experts. For the purposes of this report, an English version of the questionnaire was also produced (Supplementary File 1).
The final version of the online research questionnaire was made up of four sections:
- Demographic Variables: Seven questions regarding gender, age, academic level, and workplace characteristics.
- Life Support Training and Practice: Eight questions assessing participants’ college-based life support training, BLS and ALS certification, practice, and extracurricular preparation.
- BLS Theoretical Knowledge: Ten multiple-choice questions to measure BLS theoretical understanding.
- ALS Theoretical Knowledge: Ten multiple-choice questions to gauge ALS theoretical knowledge.
Data Collection
We used the freely available “Google Forms” tool for data collection. Participants accessed the questionnaire via a unique link shared through social media dissemination groups (Facebook and WhatsApp). The questionnaire preamble provided a brief explanation of the study’s purpose, a confidentiality assurance, and an informed consent request. All responses collected were anonymous, ensuring no personally identifiable information was solicited.
Bias
We implemented several measures to mitigate potential biases throughout the data collection and management process. To prevent duplicate responses, the “Google Forms” tool was configured to limit each IP device to a single questionnaire submission. Moreover, to reduce bias during analysis, results were independently scrutinized by researchers. Any discrepancies were collectively resolved by the research team to ensure only valid responses were included in the study’s findings.
Study Size
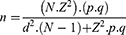
The required sample size was calculated using an equation for finite or known populations:15
Based on Ecuador’s total physician population in 2019 (N=40,230),16 and assuming a 95% confidence level (Z=95%), a 5% margin of error (d=5%), and an expected distribution of 50% for both positive (p) and negative (q) outcomes, a sample size of n=381 participants was obtained.
Data Management
Demographic variables included the work sector, classified as either public or private based on the funding source of the workplace. Single-choice responses evaluated participants’ training experiences and their perceived knowledge of basic and advanced life support.
Knowledge levels in both BLS and ALS tests were gauged using a decimal numerical rating scale, with a maximum of 10 points for each questionnaire.17 Correctly answered questions were assigned a value of 1 point, while incorrect answers received 0 points (incorrect responses did not lead to point deduction). Consequently, the highest attainable score for both the BLS and ALS questionnaires was 10.0 points, with the lowest being 0.0 points.
Statistical Analysis
For categorical variables, descriptive analysis was conducted using frequencies and percentages. Quantitative variables were analyzed through measures of central tendency (mean) and dispersion (standard deviation). Associations between the categorical variables—“sex”, “work sector”, “university training”, “BLS certification”, “ALS certification”, “belief of adequate BLS knowledge”, and “belief of adequate ALS knowledge”—and BLS and ALS knowledge scores were identified using Student’s T-test. For associations between multi-category variables such as “age”, “academic level”, “place of work”, “hospital work area”, “work experience”, “BLS practice”, “ALS practice”, and “extracurricular training” with BLS and ALS knowledge levels, one-way ANOVA analysis was used, considering “BLS score” and “ALS score” as dependent variables. Analyses with a p-value < 0.05 were deemed statistically significant. Data analysis was conducted using IBM SPSS version 26.0 software.
Ethics Approval and Consent to Participate
This research adhered to strict ethical standards, utilizing anonymized data and voluntary participation. The research protocol was reviewed and approved by the Ethics Committee of the Hospital San Francisco de Quito (HSFQ) under the code CEISH-HGSF-2023-011, ensuring compliance with ethical guidelines and standards.
Results
Demographic and Work Characteristics
A total of 385 responses from Ecuadorian physicians were collected. Of these, 56.6% (n=218) were women and 76.6% (n=295) were resident physicians. Regarding work settings, 58.2% (n=224) were public health sector workers, 52.2% (n=201) worked in first-level care, and 49.6% (n=191) in outpatient consultations. Additionally, 75.1% (n=289) had less than 3 years of work experience (Table 1).
 |
Table 1 Demographic and Work Characteristics of the Participants |
Life Support Training
The majority of participants, 81.0% (n=312), reported receiving some form of life support training during their undergraduate studies. The most common extracurricular training method was reviewing official AHA life support guides, but only 38.7% (149) did so. Regarding BLS, 71.7% (n=276) confirmed achieving BLS certification at some point, and 65.5% (n=252) believed they had sufficient theoretical BLS knowledge. However, 73.2% (n=282) had practiced BLS less than three times (Table 2).
 |
Table 2 Traits of BLS and ALS Training of the Participants |
In terms of ALS training and preparation, only half of the respondents (51.9%) reported ALS certification, a similar percentage (50.1%) believed they had adequate ALS knowledge, and 74.5% (n=149) of certified ALS physicians had practiced ALS less than three times (Table 2).
Basic Life Support (BLS) Knowledge
In terms of BLS knowledge, the overall mean score was 5.8 / 10 (±1.6 points). There were no significant differences in scores based on gender, age, or academic level of participants. Notably, those working in private sector health centers had a greater BLS knowledge score of 6.1 / 10 (±1.6 points) (p < 0.001), and physicians with less than 3 years of work experience with 5.9 / 10 (±1.5 points) (p = 0.038) (Table 3).
 |
Table 3 Mean Difference in BLS Knowledge Score According to the Characteristics of Ecuadorian Physicians |
In relation to training, it was evident that doctors who claimed to have received official certification in BLS and ALS scored higher on the BLS test, with averages of 6.0/10 ± 1.5 and 6.2/10 ± 1.5 points, respectively (p < 0.001), compared to their counterparts without such certification (Table 3).
Advanced Life Support (ALS) Knowledge
In relation to the ALS knowledge test, the average score was 4.7/10 (± 1.8 points). Physicians with less than 3 years of work experience scored marginally higher, also averaging 4.7/10 (± 1.8 points) (p = 0.038). Those working in the Intensive Care Unit (ICU) achieved a higher average score of 5.3 (± 1.6), though this difference was not statistically significant (Table 4). Finally, comparative analysis revealed that physicians’ overall score in BLS knowledge was significantly higher than in ALS knowledge (p < 0.001).
 |
Table 4 Mean Difference in ALS Knowledge Score According to the Characteristics of the Ecuadorian Physicians |
Discussion
Health professionals, particularly physicians, are expected to have adequate knowledge and skills to perform high-quality cardiopulmonary resuscitation (CPR) irrespective of their workplace.(14) To our knowledge, this study is the first to assess the theoretical knowledge of Ecuadorian physicians regarding this crucial topic in medical training. Our findings reveal that the majority of participants were young physicians with minimal work experience (less than 3 years). Moreover, the most significant group of respondents consisted of women (56.6%), which could be attributed to the current predominance of women in health-related university careers in Ecuador.18 Research also suggests that women are more likely to respond to self-administered electronic surveys.19
The academic curriculum for medical careers in Ecuador has revealed deficiencies, such as the absence of periodic updates and non-compliance with scheduled classes and syllabus.20 In the context of training in Basic and Advanced Life Support (BLS and ALS), these topics are not formally included in the academic curriculum of several Ecuadorian universities.21,22 Our research shows that 19% (n=73) of physicians reported never encountering these topics during their undergraduate education. Consequently, a majority of professionals in this study independently sought BLS (71.7%) and ALS (51.9%) certifications.
Regarding self-perception of knowledge levels among the participants, it was higher for BLS. Furthermore, knowledge measurement revealed a similar trend: the average BLS knowledge score (5.8/10 ± 1.6 points) was higher than that for ALS (4.7/10 ± 1.8 points). This discrepancy might be expected due to the greater complexity of ALS. However, our analysis revealed inadequate knowledge for both BLS and ALS among Ecuadorian doctors, as the average score of correct answers did not reach 60% of the total score (10.0 points) in any of the tests. These findings are particularly concerning given the critical importance of these skills in clinical practice and are unprecedented; similar knowledge gaps have been observed among Nigerian, Greek, Thai, Indian, Ethiopian, and Arab physicians.13,23–27
Exploring the influence of participant characteristics on knowledge levels yielded intriguing results. While education during college showed no correlation with better BLS or ALS knowledge, those with certificates in BLS and ALS scored higher on BLS tests (p < 0.001). However, this correlation was absent in ALS test scores, aligning with findings by Good et al, where 60 American healthcare professionals, despite ALS certification, showed poor competence in different settings.28 Thus, establishing a direct relationship between certification and high knowledge levels in life support is challenging based on our findings. Contrastingly, studies in Ethiopia and Nepal indicated that prior training significantly improved CPR knowledge.29,30 A potential explanation for these discrepancies might be the effect of time on knowledge retention; CPR knowledge scores have been shown to decline after six months post-training.31
Sources of extracurricular preparation among participants showed higher levels of BLS knowledge (p = 0.004) among those using resources like the AHA Official Guides to Life Support and video materials. Physicians consulting these guidelines better understand theoretical and practical aspects of life support, aiding in the retention of algorithms and guidelines.29
Regarding work experience, less experience correlated with greater average knowledge in both BLS and ALS (p < 0.05) among our participants. This trend, though not fully understood, mirrors findings in other studies. For instance, a Pakistani study found that younger doctors scored higher on a BLS knowledge questionnaire,32 and an Indian study showed that doctors with less than five years of experience had greater BLS and ALS knowledge.25 Conversely, Irfan et al observed that greater experience among Pakistani physicians correlated with better BLS knowledge,14 aligning with Sánchez et al’s findings among more experienced Spanish doctors having more certifications and hence greater CPR knowledge.33 Despite these contradictions, we hypothesize that the difference in our study might be because younger and non-specialized Ecuadorian doctors are more likely to work with critically ill patients, mainly in emergency departments. As physicians specialize, their interaction with emergency services decreases.32
Furthermore, while not part of formal academic training, factors like the work environment must be considered in doctors’ knowledge acquisition. Physicians in private healthcare facilities scored higher on BLS knowledge than those in the public sector (p < 0.001). This could be due to increased training opportunities in life support in the private sector. However, it’s notable that physicians working in emergency departments did not significantly excel in BLS and ALS knowledge compared to others. This finding is surprising because Adal and Emishaw reported higher ALS knowledge levels among physicians working in the emergency department for 10 years or more.26
In Ecuador, and across much of South America, BLS and ALS certifications are mandatory for most healthcare jobs. Many new graduates hold these certifications, yet our findings suggest that certification does not guarantee acceptable knowledge levels, which is concerning. Knowledge acquisition is multifaceted, and identifying factors that directly influence life support knowledge levels is complex. Nevertheless, we believe that formal training, certification, and regular recertification are crucial to enhancing physicians’ knowledge and competency in basic and advanced life support. This is particularly important in Ecuador and other South American countries, where emergency response team efficiency may not match that of developed countries.34,35 Longer wait times for emergency services significantly impact patient outcomes, emphasizing the critical role of well-trained physicians in life-threatening situations. A physician’s knowledge in basic and advanced life support can be life-saving in these crucial moments.36
Therefore, we urge primary healthcare stakeholders, including national health authorities, universities, and hospitals, to develop accreditation policies and regular training programs. By doing so, we aim to create a healthcare system staffed with well-trained and qualified physicians, capable of providing life-saving interventions when most needed. This goal is not only pertinent to Ecuador but is also fundamental for the entire South American region, ultimately fostering a more resilient healthcare system capable of delivering better patient outcomes.
Strengths and Limitations
This study has several limitations that may affect the robustness of its conclusions. Firstly, its self-report design inherently introduces a risk of selection bias, since physicians with a specific interest in life support and emergency medicine might have been more likely to participate. Secondly, the evaluation system used to assess participants’ knowledge, developed specifically for this study, may impact the generalizability of the findings. However, rigorous steps were taken to validate this instrument, including expert review to ensure equal weighting of questions and use of a decimal-type numerical rating scale considering each question separately.
The questionnaire itself is another limitation, as it only measures theoretical knowledge of basic and advanced life support. This represents a potential direction for future research to incorporate practical skill assessment. To prevent duplicate responses, the survey, using “Google Forms”, allowed only one response per device, potentially restricting multiple legitimate respondents sharing a device.
Lastly, social desirability bias could have played a role due to concerns over response anonymity. While we emphasized the anonymity of data collected and the importance of honesty in response, this may not have completely mitigated this bias.
Conclusions
Ecuadorian physicians demonstrate a level of theoretical knowledge in basic and advanced life support that is generally deficient. The knowledge of basic life support was significantly higher than that of advanced life support, albeit the differences were not as expected. The most influential factor on knowledge levels was having less than 3 years of work experience. However, the critical importance of robust knowledge in both basic and advanced life support across all scenarios is irrefutable. To address this, key stakeholders in academic training, such as universities and healthcare facilities, should prioritize promoting regular training and academic updates on life support.
Data Sharing Statement
The dataset of this research can be freely accessed at the following DOI of the “figshare” online repository: 10.6084/m9.figshare.23264654. The summary of the questionnaire and its results are included in this article.
Acknowledgments
We express our gratitude to all participants who voluntarily participated in this study. We also extend our thanks to Universidad de las Américas for financially supporting the publication of this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. González-Inciarte ME, López JM, Luisa G, et al. Evaluación del conocimiento sobre reanimación cardiopulmonar pediátrica en residentes del tercer año de pediatría [Knowledge Assessment in Pediatric CPR by Pediatric Third Year Residents]. Archivos Venezolanos de Puericultura y Pediatría. 2014;77:170–177. Spanish.
2. Gadipelly S, Neshangi S. Changing guidelines of cardiopulmonary resuscitation and basic life support for general dental practitioners and oral and maxillofacial surgeons. J Maxillofac Oral Surg. 2015;14(2):182–187. doi:10.1007/s12663-014-0649-1
3. Aranzábal-Alegría G, Verastegui-Díaz A, Quiñones-Laveriano DM, et al. Factors influencing the level of knowledge of cardiopulmonary resuscitation in hospitals in Peru. Rev Colomb Anestesiol. 2017;45:114–121. doi:10.1016/j.rcae.2017.01.001
4. World Health Organization. Enfermedades cardiovasculares [Cardiovascular diseases]; 2017. Available from: https://www.who.int/es/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
5. Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–2406. doi:10.1097/CCM.0b013e3182257459
6. Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi:10.1161/CIR.0000000000000916
7. Gazmuri RJ. Reanimación cardiopulmonar intra-hospitalaria del paciente adulto [In-hospital cardiopulmonary resuscitation of the adult patient]. RevMédClín Las Condes. 2017;28:228–238. Spanish. doi:10.1016/j.rmclc.2017.04.010
8. Cooper JA, Cooper JD, Cooper JM. Cardiopulmonary resuscitation: history, current practice, and future direction. Circulation. 2006;114:2839–2849. doi:10.1161/CIRCULATIONAHA.106.610907
9. Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital. Circulation. 2013;128:417–435. doi:10.1161/CIR.0b013e31829d8654
10. Field JM, Hazinski MF, Sayre MR, et al. Part 1: executive summary: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S640–S656. doi:10.1161/CIRCULATIONAHA.110.970889
11. Avisar L, Shiyovich A, Aharonson-Daniel L, Nesher L. Cardiopulmonary resuscitation skills retention and self-confidence of preclinical medical students. Isr Med Assoc J. 2013;15:622–627.
12. Toubasi S, Alosta MR, Darawad MW, Demeh W. Impact of simulation training on Jordanian nurses’ performance of basic life support skills: a pilot study. Nurse Educ Today. 2015;35(9):999–1003. doi:10.1016/j.nedt.2015.03.017
13. Passali C, Pantazopoulos I, Dontas I, et al. Evaluation of nurses’ and doctors’ knowledge of basic & advanced life support resuscitation guidelines. Nurse Educ Pract. 2011;11:365–369. doi:10.1016/j.nepr.2011.03.010
14. Irfan B, Zahid I, Khan MS, et al. Current state of knowledge of basic life support in health professionals of the largest city in Pakistan: a cross-sectional study. BMC Health Serv Res. 2019;19:865. doi:10.1186/s12913-019-4676-y
15. García-García JA, Reding-Bernal A, López-Alvarenga JC. Cálculo del tamaño de la muestra en investigación en educación médica [Sample size calculation in medical education research]. Investigación en Educación Médica. 2013;2(8):217–224. Spanish. doi:10.1016/S2007-5057(13)72715-7
16. Instituto Nacional de Estadística y Censos. Registro Estadístico de Recursos y Actividades de Salud [Statistical Registry of Health Resources and Activities]. Instituto Nacional de Estadística y Censos; 2022. Available from: https://www.ecuadorencifras.gob.ec/actividades-y-recursos-de-salud/.
17. Martínez-Rojas JG. Las rúbricas en la evaluación escolar: su construcción y su uso [Rubrics in school evaluation: their construction and use]. Adv Med. 2008;6:129–138. Spanish.
18. Ferreira Salazar C, García García K, Macías Leiva L, Pérez Avellaneda A Mujeres y Hombres del Ecuador en cifras III serio de información estratégica [Women and Men of Ecuador in Figures III strategic information series]. Instituto Nacional de Estadística y Censos. ONU Mujeres; 2012. Available from: https://www.ecuadorencifras.gob.ec/wp-content/descargas/Libros/Socioeconomico/Mujeres_y_Hombres_del_Ecuador_en_Cifras_III.pdf.
19. Smith WG. Does gender influence online survey participation?: a record-linkage analysis of university faculty online survey response behavior. ERIC Inst Educ Sci. 2008;2008:1–21.
20. Izquierdo-Condoy JS, Simbaña-Rivera K, Nati-Castillo HA, et al. How much do Latin American medical students know about radiology? Latin-American multicenter cross-sectional study. Med Educ Online. 2023;28(1):2173044. doi:10.1080/10872981.2023.2173044
21. Cabrera Proaño L, Cazar García J. Hacia una educación de excelencia: el rediseño curricular de medicina aprobado en 2017 genera nuevos cambios [Towards an education of excellence: the redesign of the curricular redesign of medicine approved in 2017 generates new changes]. Rev Fac Cien Med. 2018;43:1. Spanish.
22. Universidad Católica de Santiago de Guayaquil. Carrera de Medicina [Medicine Career]. Carrera de medicina - Información de la Carrera; 2023. Spanish. https://www.ucsg.edu.ec/cme/c044046/.
23. Akinbodewa A, Gbala M, Ige O, Akinkunmi F, Odanye A. Knowledge of basic life support among doctors and nurses attending a refresher course in a teaching hospital in Southwest Nigeria: knowledge of basic life support. Niger Med J. 2022;63:304–311.
24. Boonmak P, Boonmak S, Chongarunngamsang W, Maharungruengrat K. Advanced cardiac life support knowledge among medical staff and residents in university hospital. Srinagarind Med J. 2009;24(4):296–301.
25. Nambiar M, Nedungalaparambil NM, Aslesh OP. Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala. World J Emerg Med. 2016;7:263–269. doi:10.5847/wjem.j.1920-8642.2016.04.004
26. Adal O, Emishaw S. Knowledge and attitude of healthcare workers toward advanced cardiac life support in Felege Hiwot Referral Hospital, Bahir Dar, Ethiopia, 2022. SAGE Open Med. 2023;11:20503121221150101. doi:10.1177/20503121221150101
27. Fatani AA, Johani NA, Ibrahim AM. Basic life support knowledge of family medicine residents at joint program of family medicine in Jeddah Saudi Arabia, 2017. Int J Community Med Public Health. 2019;6(6):2372–2377. doi:10.18203/2394-6040.ijcmph20192227
28. Good JJ, Rabener MJ. ACLS interventional skills: are we as good as we should be? J Am Acad Phys Assist. 2021;34:40–45. doi:10.1097/01.JAA.0000735764.43931.0c
29. Mersha AT, Egzi AHKG, Tawuye HY, Endalew NS. Factors associated with knowledge and attitude towards adult cardiopulmonary resuscitation among healthcare professionals at the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia: an institutional-based cross-sectional study. BMJ Open. 2020;10:e037416. doi:10.1136/bmjopen-2020-037416
30. Roshana S, Kh B, Rm P, Mw S. Basic life support: knowledge and attitude of medical/paramedical professionals. World J Emerg Med. 2012;3:141–145. doi:10.5847/wjem.j.issn.1920-8642.2012.02.011
31. Singhal Y, Bhatnagar R, Lal B, Paliwal B. Knowledge, attitudes, and practices of medical internship students regarding disaster preparedness at a tertiary-care hospital of Udaipur, Rajasthan, India. Int J Med Sci Public Health. 2016;5:1613. doi:10.5455/ijmsph.2016.25112015263
32. Zamir Q, Nadeem A, Rizvi AH. Awareness of cardiopulmonary resuscitation in medical-students and doctors in Rawalpindi-Islamabad, Pakistan. J Pak Med Assoc. 2012;62:1361–1364.
33. Sánchez-García AB, Fernández-Alemán JL, Pérez NA, Hernández IH, Valverde RN, Castro DR. Valoración del nivel de conocimientos y su adecuación en materia de RCP en el personal sanitario de los servicios de urgencias hospitalarios de la Comunidad Autónoma de la Región de Murcia [Assessment of the knowledge level and its relevance in terms of CPR in medical personnel of the hospital emergency medical system of the Autonomous Community of the Region of Murcia]. Enfermeria Glob. 2015;14:230–260. Spanish. doi:10.6018/eglobal.14.3.197791
34. Litewka SG, Heitman E. Latin American healthcare systems in times of pandemic. Dev World Bioeth. 2020;20:69–73. doi:10.1111/dewb.12262
35. Benítez MA, Velasco C, Sequeira AR, Henríquez J, Menezes FM, Paolucci F. Responses to COVID-19 in five Latin American countries. Health Policy Technol. 2020;9:525–559. doi:10.1016/j.hlpt.2020.08.014
36. Graham R, McCoy MA, Schultz AM; Directions C on the T of CACS and F, Policy B on HS, Medicine I of. Emergency medical services response to cardiac arrest. Strategies to improve cardiac arrest survival: a time to act. National Academies Press (US); 2015. Available from: https://www.ncbi.nlm.nih.gov/books/NBK321505/.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.